Breast cancer screening
"It changed my life"

“This mammogram , it changed my life…There was no history of breast cancer in my family, so I didn’t think it applied to me…Because of that mammogram, I’m here today to share this time with my husband, with my family.”
"I thank God for getting this"

“I thank God for getting this done because things could have turned out a lot differently for me…If it had not been for me getting that mammogram, my odds would be very different right now…I have family that I want to see and I have things that I have yet to do.”
In 2016, Charlotte Radiology of North Carolina, a large radiology group that currently owns and operates 17 breast centers and a mobile breast center program, asked 14 breast cancer survivors about how important early detection with mammograms was for them and whether women should wait until age 50 (which was the recommendation at that time) before beginning regular screening.
An emotional 5-minute video from Charlotte Radiology.
Eary detection meant no radiation or chemotherapy

“I had my mammogram yearly, so I didn’t have radiation or chemotherapy because of early detection.
"I would probably be dead"

“If I had not had a mammogram by the age of 40, I would probably be dead right now.”
"If it wasn't for that routine mammogram..."
“I tell everyone that a mammogram saved my life. If it wasn’t for that routine mammogram that I had every year, I don’t know when I would have been able to find the cancer. It was so far back on my chest wall that it was already stage 2 and you couldn’t feel it at all. I encourage every women to get a mammogram.”
A 1-minute video from Sarasota Memorial Health Care System.
"My mammogram saved my sister's life"
“Because I was diagnosed with breast cancer early, my younger sister went in for what was a routine screening. She was not symptomatic, there was no lump that she could feel. The mammogram found a lump and it saved her life…”
“She’s going on living a fruitful, prosperous and wonderful life because she went in for a mammogram. A mammogram is more frightening when we talk about it than it is to actually take it. I’ve had many and I will say this to the person who’s afraid of the mammogram: I’d be afraid not to have it.”
A 2-minute video from Johns Hopkins Medicine.
A young boy pulls a wagon full of gifts to a clinic. Watch until the end to see the message on his sign.
A 1-minute video from the American Cancer Society.
Guidelines
National Comprehensive Cancer Network (2022)
Women should undergo a risk assessment for developing breast cancer starting at age 25. Increased risk is based on a number of factors including age and family history of certain cancers—including ovarian and pancreatic cancer, not just breast cancer. Average risk means a woman has no known genetic or family history that suggests an increased risk of developing breast cancer.
From ages 25 to 39, a woman with average risk should see a healthcare professional for a checkup every 1 to 3 years, which should include a breast cancer risk assessment and, if not recently done, a breast exam.
At age 40 and older, a woman with average risk should see a healthcare professional for a checkup every year, which should include an ongoing breast cancer risk assessment and, if not recently done, a breast exam. She should have an annual screening mammogram. If available, a tomosynthesis (3D mammogram) is recommended.
A woman at increased risk for breast cancer should see a healthcare professional at least once a year and may be asked to see one more often.
Source: Breast Cancer Screening and Diagnosis (National Comprehensive Cancer Network, 2022)
The National Comprehensive Cancer Network (NCCN) is a not-for-profit alliance of leading cancer centers devoted to patient care, research, and education.
American Cancer Society (2022)
A woman is considered to be at average risk if she doesn’t have a personal history of breast cancer, a strong family history of breast cancer, or a genetic mutation known to increase risk of breast cancer (such as in a BRCA gene), and has not had chest radiation therapy before the age of 30.
Women ages 21-39: All women should know how their breasts normally look and feel and report any changes to a health care provider right away. Find out if you are at higher than average risk for breast cancer. If you are, talk to a health care provider about when you need to start getting mammograms or other screening tests. If not, then testing is not needed at this time.
Women at average risk between 40 and 44 have the choice to start annual breast cancer screening with mammograms if they wish to do so.
Women ages 45-54: should get mammograms every year.
Women ages 55+: should switch to getting mammograms every 2 years, or can continue to get one every year. Screening should continue as long as a woman is in good health and is expected to live at least 10 more years.
Most women at high risk should begin screening with MRI and mammograms when they are 30 and continue for as long as they are in good health. But this is a decision that should be made with a woman’s health care providers, taking into account her personal circumstances and preferences.
Clinical breast exams are not recommended for breast cancer screening among average-risk women at any age. Women should be able to choose between 2D and 3D mammography if they or their doctor believes one would be more appropriate, and that out-of-pocket costs should not be a barrier to having either one.
Sources: American Cancer Society Recommendations for the Early Detection of Breast Cancer (2022) and Cancer Screening Guidelines by Age.
American College of Radiology and the Society of Breast Imaging (2023)
New American College of Radiology (ACR) breast cancer screening guidelines now call for all women — particularly Black and Ashkenazi Jewish women — to have risk assessment by age 25 to determine if screening earlier than age 40 is needed.
The ACR continues to recommend annual screening starting at age 40 for women of average risk.
For women at higher-than-average risk of breast cancer, the ACR recommends annual digital mammography, beginning between ages 25 and 40, and supplemental screening, depending on risk, with breast MRI as the supplemental method of choice.
Sources: New ACR Breast Cancer Screening Guidelines call for earlier and more-intensive screening for high-risk women (May 3, 2023) and Breast Cancer Screening for Women at Higher-than-Average Risk:Updated Recommendations from the ACR (2023)
U.S. Preventive Services Task Force (2023)
After years of promising a revision of its breast cancer screening recommendations, the U.S. Preventive Services Task Force in May 2023 announced that it “now recommends that all women get screened for breast cancer every other year starting at age 40… More research is needed on whether or not women with dense breasts should have additional screening with breast ultrasound or MRI, and on the benefits and harms of screening in women older than 75. The use of the term women in this draft recommendation includes cisgender women and other people assigned female at birth…
“This draft recommendation applies to women at average risk of breast cancer. This includes people with a family history of breast cancer and people who have other risk factors, such as having dense breasts. It does not apply to people who have a personal history of breast cancer, who are at very high risk of breast cancer due to certain genetic markers or a history of high-dose radiation therapy to their chest at a young age, or who have had a high risk lesion on previous biopsies. Anyone concerned with their breast health should talk with their healthcare professional.”
Source: Task Force Issues Draft Recommendation Statement on Screening for Breast Cancer (May 9, 2023)
Note: The U.S. Preventive Services Task Force is an independent, volunteer panel of national experts in disease prevention and evidence-based medicine who make evidence-based recommendations about clinical preventive services.
Recent news about breast cancer screening
Waiting until 45 or 50 to be screened for breast cancer "is a disaster for women of color"

Minority women are 72% more likely to be diagnosed with invasive breast cancer under the age of 50. Minority women under 50 years old are 58% more likely to present with advanced cancer and are 127% more likely to die than white women from breast cancer.
“I think it really points to the fact that we are failing Black women,” says Debra Monticciolo, MD, former president of the American College of Radiology.
“Waiting until 45 or 50 [to be screened] is not good for any woman, but it’s a disaster for women of color, especially Black women.”
Source: “Improvements needed in breast cancer screening for Black women”
Getting a Mammogram
Locating a Provider
Contact the National Cancer Institute (1-800-4-CANCER) or the American College of Radiology (1-800-227-5463) to find a certified mammography provider. You may want to look for a facility that can do MRI, ultrasound, or other imaging procedures the same day if it’s necessary to get a more precise look.
Source: breastcancer.org
Insurance Coverage
Medicare, Medicaid and most insurance companies cover the cost of mammograms.Since September 2010, the Affordable Care Act has required all new health insurance plans to cover screening mammograms every 1-2 years for women ages 40 and older, with no out-of-pocket costs (co-payments or co-insurance).
Source: Susan G. Komen
For the Uninsured
The Komen Breast Care Helpline can help you find low-cost breast cancer screening in your area. Call the helpline at 1-877 GO KOMEN (1-877-465-6636) Monday through Friday from 9:00 a.m. to 10:00 p.m. ET.
The National Breast and Cervical Cancer Early Detection Program ((1-888-842-6355) provides access to breast cancer screening to low-income, uninsured and underinsured women ages 40-64. It also provides access to diagnostic testing if results are abnormal, and referrals to treatment if breast cancer is diagnosed.
Source: Susan G. Komen
Questions about Mammography
What is a mammogram? What is breast tomosynthesis? who should get a mammogram?
How can I prepare for a mammogram? What happens during my mammogram? Does a mammogram hurt? What are the risks of getting a mammogram?
How will I get my results?
A 4-minute video from the Department of Radiology at Massachusetts General Hospital.
Questions to ask
“Younger women tend to have denser breasts, but mammograms are not the best when you have dense breast tissue,” says Regina Hampton, MD, breast cancer surgeon at Luminis Health in Maryland.
“Mammograms get better as women get older and breasts become less dense. So, it’s really important for patients to look at their report and see what it’s saying about breast density.”
A 2-minute video from the Patient Empowerment Network.
Your First Mammogram
First of all, wear a two-piece outfit so you only have to remove your top. Give your beauty products the day off.
Think of the X-ray machine as your friend. You’ll give it a quick hug as it compresses your breast between two flat paddles. The machine will use a safe, low-dose X-ray to take multiple images of each breast.
The procedure takes only about 20 seconds per image. And that’s it!
A 1-minute video from MD Anderson Cancer Center.
What to know about tomosynthesis
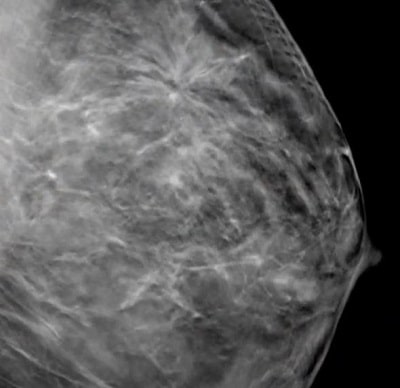
Tomosynthesis is a type of mammography. It helps screen for breast cancer, and because it involves relatively new technology, it is only available in some hospitals.
Standard mammograms and tomosynthesis both use X-rays to create an image of the breast, but while the image from a mammogram is 2D, the image from tomosynthesis is 3D.
Because it produces a 3D image rather than a flat one, tomosynthesis give more accurate information about changes in the breast, including whether they warrant further evaluation.
See “What to know about tomosynthesis for breast cancer” by Hannah Nichols on the Medical News Today website (January 12, 2022)

"If a patient waits until something is felt, it may be too late already."
Oprah: Make screening "a birthday health-filled well-being celebration"
“It’s time to normalize asking one another, ‘When’s the last time you had a mammogram’?”
“Here’s an idea: schedule that appointment together if that helps you follow through. One of the things I’ve learned is to make it a birthday, health-filled, well-being celebration! If you schedule it every year around your birthday, that signals you’re taking care of yourself and taking care of your girls!”
A 2-minute video from Hologic, Inc.
Four ministers in Pittsburgh area urge women to get screened for breast cancer
“Our female friends and relatives definitely need to get tested. Do it for your family.”
“I think that most women think they’re too young and they think it won’t happen to them. I was diagnosed with breast cancer. I never thought it would have happened to me.”
“There are too many people dying in the African American community of treatable diseases. With examinations and testing, we can really extend lives. Get a mammogram.”
“I thought they’re looking so they can find something, not realizing the truth is they’re making sure everything is OK. Please, please, get screened for breast cancer.”
Breast Self-Exams

There is very little evidence that regular physical breast exams done by either a health professional or by women themselves help find breast cancer early when women also get screening mammograms.
Most often when breast cancer is detected because of symptoms (such as a lump), a woman discovers the symptom during usual activities such as bathing or dressing. Women should be familiar with how their breasts normally look and feel and should report any changes to a health care provider right away.
This does not mean that these exams should never be done. In some situations, particularly for women at higher than average risk, health care providers may still offer clinical breast exams along with counseling about risk and early detection. And some women might still be more comfortable doing regular self-exams as a way to keep track of how their breasts look and feel.
Source: American Cancer Society Recommendations for the Early Detection of Breast Cancer

Breastcancer.org still believes that breast self-examination is a useful and important screening tool, especially when used in combination with regular physical exams by a doctor, mammography, and in some cases ultrasound and/or MRI.
Breast self-exam is a convenient, no-cost tool that you can use on a regular basis and at any age. We recommend that all women routinely perform breast self-exams as part of their overall breast cancer screening strategy.
How to do a breast self-exam: The five steps
(breastcancer.org)