Breast Cancer Disparity Facts
- more likely to be diagnosed with breast cancer at an earlier age
- more likely to be diagnosed with aggressive breast cancer
- more likely to be diagnosed with more advanced stage of breast cancer
- less likely to receive optimal treatment
- much more likely to die of breast cancer
- more likely to be diagnosed with larger and more difficult to treat tumors
- more likely to be diagnosed with advanced stages of breast cancer
- less likely to receive optimal treatment

W=White 137.6, B=Black 129.6,
NA=Native American 111.3, A=Asian/Pacific Islander 106.9, H=Hispanic 99.9
Source: National Cancer Institute Cancer
Stat Facts: Female Breast Cancer
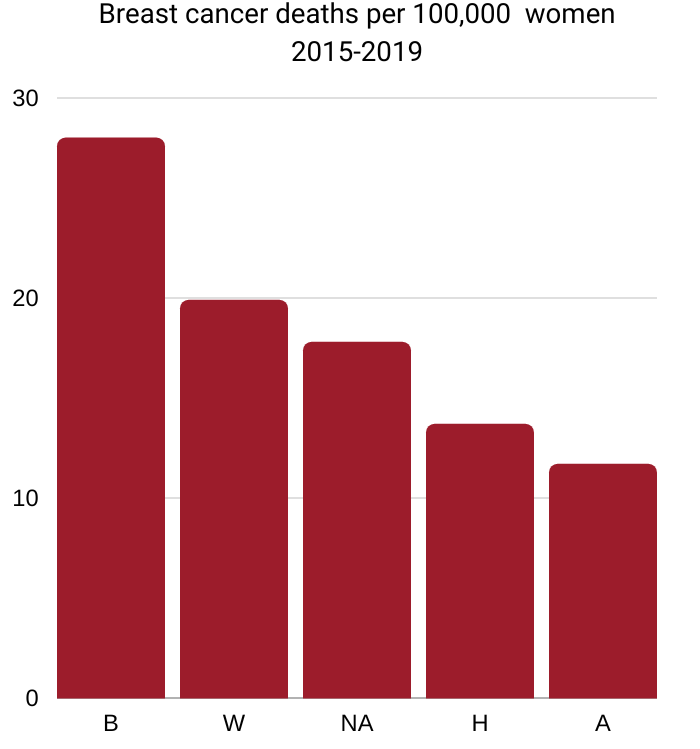
B=Black 28.0, W=White 19.9,
NA=Native American 17.8, H=Hispanic 13.7, A=Asian/Pacific Islander 11.7
Source: National Cancer Institute Cancer
Stat Facts: Female Breast Cancer
Incidence
Black women. Breast cancer is the most commonly diagnosed cancer among Black women. Similar to the pattern among White women, incidence rates among Black women increased rapidly during much of the 1980s, largely due to increased detection of asymptomatic lesions through newly introduced mammography screening. Recently, increases have slowed and are approaching stabilization in Black women, in contrast to continued increases among White women.
During 2014-2018, the overall breast cancer incidence rate was 127.1 cases per 100,000 in Black women compared to 132.5 in White women, although rates are higher among Black women younger than 40 years of age.
As a result of higher rates among Black women younger than 40 years of age and also because of shorter life expectancy, the median age of diagnosis is younger for Black women, 60 years compared to 64 for White women.
Black breast cancer survivors also have a much higher likelihood of being diagnosed with new cancers because young-onset receptor negative tumors, such as TNBC, are associated with a higher risk of subsequent malignancies than other breast cancer subtypes.
During 2014-2018, the overall breast cancer incidence rate was slightly lower in Black women compared to White women (127 versus 132 per 100,000 cases, respectively). However, it is concerning that, among women who are younger than 40 years, the breast cancer incidence rates are higher among Black women compared to White women.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022
Black men. Breast cancer has a higher prevalence among Black men. Overall, Black men have 44-52 percent higher risk of developing breast cancer compared to White men Black men are also more than twice as likely as White men to develop highly aggressive forms of breast cancer, such as triple negative breast cancer.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022
Although breast cancer in men is rare, Black men have a higher incidence of all breast cancer subtypes than White men, including a two-fold higher risk of TNBC.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Hispanic women. Breast cancer is the most commonly diagnosed cancer among Hispanic women. The incidence rate increased in Hispanic women from 2006 to 2015 (0.4% annually) while remaining stable in whites. Within the Hispanic population, studies have shown that the risk of breast cancer is even lower in those who are foreign-born.
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020. Atlanta: American Cancer Society, 2018.
Hispanics have a lower rate of breast cancer compared with Whites. Genetic ancestry studies have demonstrated that the risk of breast cancer is lower in Hispanic women if more of their genetic makeup comes from a higher proportion of Indigenous American ancestry, but increases if more of their genetic makeup comes from European ancestry.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022.
Native Hawaiian women. Native Hawaiian women had the highest incidence and mortality from breast cancer compared to any other racial or ethnic group in Hawaii.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022.
Native Hawaiian and Pacific Islander (NHPI) women diagnosed with breast cancer have higher rates of Inflammatory Breast Cancer (IBC), the most aggressive form of breast cancer compared to other racial/ethnic populations in Hawaiʻi.
Source: Improving breast cancer outcomes for Native Hawaiians, Pacific Islanders (2023)
Tumor subtypes
Triple Negative Breast Cancer. Black women are twice as likely as women of other racial and ethnic groups in the US to be diagnosed with triple negative breast cancer (TNBC). Women with TNBC generally have poorer outcomes because of few effective treatments. Nevertheless, Black women are still about 30% more likely to die from these tumors than White women, partly because of lesser rates of surgery and chemotherapy.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Inflammatory Breast Cancer. Black women are also 72 percent more likely than White women to be diagnosed with inflammatory breast cancer, a rare but aggressive subtype. Black women are diagnosed with this cancer at an average of four years younger than White women. And Black women die an average of one and one-half years earlier than White women with the disease.
Source: Incidence and survival of inflammatory breast cancer between 1973 and 2015 in the SEER database (2020).
Reasons for the Black-White variation in subtype distribution remain unclear, but do not appear to be completely explained by the differences in the prevalence of inherited genetic mutations.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Hispanic women. Hispanic women are more likely to be diagnosed with tumors that are larger and are hormone receptor negative, both of which are more difficult to treat.
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020. Atlanta: American Cancer Society, 2018.
Screening
Black women. Black women are less likely than White women to have their imaging performed at a facility with the most current technology, such as digital breast tomosynthesis, and also have a longer time between abnormal results and follow-up.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Stage at diagnosis
Black women. Despite similar self-reported screening prevalence, only 57% of breast cancers in Black women are diagnosed at a local stage compared to 67% in White women. A recent study found that over half of this disparity is due to differences in insurance coverage.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Hispanic women. Breast cancer is less likely to be diagnosed at a local stage in Hispanic women than in non-Hispanic white women, even after accounting for differences in age, socioeconomic status, and method of detection. During 2011-2015, 57% of breast cancers among Hispanic women were diagnosed at a local stage, compared to 65% among non-Hispanic white women. Lower rates of mammography utilization and delayed follow-up of abnormal screening results or self-discovered breast abnormalities among Hispanic women likely contribute to this difference.
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020. Atlanta: American Cancer Society, 2018.
Clinical trials
Black and Hispanic women are under-represented in clinical trials that look at biomarkers which can help identify appropriate personalized treatments. White and Asian women are over-represented in these trials.
Source: “Racial and Ethnic Disparities Among Participants in Precision Oncology Clinical Studies” by Christopher M. Aldrighetti et al. (November 8, 2021).
Treatment
Hispanic women. Hispanic women are less likely than white women to receive appropriate and timely breast cancer treatment.
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020. Atlanta: American Cancer Society, 2018.
5-year survival
Black women. The overall 5-year relative survival rate for breast cancers diagnosed in 2011-2017 was 82% for Black women compared to 92% for White women, partly due to more advanced stage at diagnosis for Black women.
Black women have lower survival at every stage of disease, largely because of less access to high-quality health care, including receipt of care at low-resourced and/or unaccredited facilities. The greater burden of TNBC in Black women also contributes to disparate outcomes, although research suggests that Black women have lower survival than White women regardless of molecular subtype.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Mortality
Black women. Breast cancer is the leading cause of cancer death among Black women, with an estimated 6,800 deaths expected to occur among Black women in 2022. Improvements in early detection and screening have led to a decrease in mortality for Black women since 1990. However, because the decline began later and was slower compared to White women, this progress led to a widening disparity that peaked in 2011-2012.
From 2010 to 2019, mortality rates continued to decrease in Black and White women by a little over 1% per year; from 1990, the breast cancer death rate dropped by 30% in Black women versus 41% in White women. Breast cancer death rates in the most recent time period (2015-2019) are 41% higher in Black women compared to White women. This racial disparity is largely due to more advanced stage at diagnosis; higher prevalence of obesity, other comorbidities, and unfavorable tumor characteristics, such as TNBC; and less access to high-quality treatment, likely due to financial barriers.
Lack of private insurance and unfavorable tumor characteristics explain one-third and one-fifth of the disparity, respectively among women with early-stage disease younger than 65 years of age. Although there are some differences between Black and White women in the prevalence of genetic variations, they do not appear to explain the survival gap.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Hispanic women. Breast cancer is the leading cause of cancer death among Hispanic women. From 2007 to 2016, breast cancer death rates decreased by 1.1% per year among Hispanic women (versus a decline of 1.8% per year among white women). However, declines in Hispanic women younger than 50 years of age appear to have stabilized in recent years.
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020. Atlanta: American Cancer Society, 2018.
More Black Women Die from Breast Cancer Than Any Other Cancer

A diagnosis of breast cancer can be devastating for anyone. It’s even more alarming to know that the color of someone’s skin can be a factor in their survival. There are many reasons for the disparity: There are challenges in accessing healthcare. Black women are more likely to be living in poverty and be under- or uninsured. There are high levels of medical mistrust, which worsens health outcomes. Systemic racism is being recognized as a determinant of health.
When healthcare professionals understand the barriers that Black women may face in diagnosis and treatment, change can start to happen to improve outcomes for Black women with breast cancer.
Source: “More Black Women Die from Breast Cancer Than Any Other Cancer” by Carly Werner (2022)
Why the Disparities in Dying?
“It is extremely interesting to me that you have similar incidence rates, but the mortality rate is different and you wonder why is that?” asks Shaina Rozell, MD, an Illinois cancer physician.
“A lot of it has to do with the time in which women actually seek care. African American women are seeking care at later stages.”
A 3-minute video from MD Newslines.
Why Is This Happening?
“Here’s some research that may surprise you and really hits home for me,” says television journalist Robin Roberts.
“African American women are more likely to die from breast cancer.
Why is this happening? And what can be done about it? We take a closer look.”
A 6-minute video from WebMD
Aggressive Cancer
“We see that African American breast cancer patients tend to be diagnosed at younger ages on average,” says Lisa Newman, MD, chief of Breast Surgery at New York-Presbyterian/Weill Cornell Medical Center in New York.
“Also very concerning is the higher rates of biologically aggressive cancer in African American women.”
A 2-minute video from OncLiveTV.
"Lack of health insurance is a barrier"
“Lack of health insurance is a barrier in receiving timely screening to detect breast cancer early on and is a big reason that we see higher breast cancer death rates in Black women,” says Oluchi Oke, MD, an oncologist at the University of Texas MD Anderson Cancer Center.
 “The most well-known study looked at five factors that may impact the difference in outcome between Black versus Caucasian women with stage 1-3 breast cancer, including demographics, characteristics of cancer, comorbidities, health insurance, and type of treatment.”
“The most well-known study looked at five factors that may impact the difference in outcome between Black versus Caucasian women with stage 1-3 breast cancer, including demographics, characteristics of cancer, comorbidities, health insurance, and type of treatment.”
“The difference in health insurance was the biggest contributor to the difference in death rate for each group. Almost three times as many Black women were uninsured compared to white women, and 35% of the excess risk of death from breast cancer in Black women compared with white women was due to a difference in health insurance. The type of tumor also contributed to the increased risk of death, but not as significantly as the lack of insurance contributed.”
See “An Expert Explains How Racial Disparities in Breast Cancer Care Contribute to Poor Outcomes for Black Women And how to close the health care gap” by Nina Bahadur on the Self magazine website (October 25, 2021)
Six drivers of breast cancer disparities

The Susan G. Komen Foundation conducted focus groups in 10 major metropolitan areas to understand the many barriers Black women face in preventing, treating and surviving breast cancer. The research identified several trends that exist to varying degrees in each metropolitan area.
Source: “Susan G. Komen Launches “Stand For H.E.R.”, A Health Equity Revolution To Improve Breast Cancer Outcomes In The Black Community” (August 4, 2021)
1. Black women often feel ignored or met with disapproval by heath care providers and others in the health care system. Some experience harsh, uncompassionate and unnecessarily painful treatment.
2. Health care providers often do not grasp the barriers some Black women face, including lack of access to healthy foods and economic insecurity.
3. The quality of health care is segregated. High-quality institutions are located in predominately white neighborhoods, while Black communities are often supported by community clinics that often do not meet quality standards of care.
4. Many health care facilities that provide quality care do not accept Medicaid, Medicare or other lower-cost health exchange plans. Black women on these plans often feel discriminated against even when the hospital accepts the insurance.
5. Many cannot afford to travel to high-quality care locations or are concerned about losing their job if they take time off for appointments.
6. Barriers plague access to genetic counseling and testing services in the Black community, which are valuable for those with a family health history of cancers.
Disparity in breast cancer deaths emerged in the 1980s

It may come as a surprise that before 1980, breast-cancer mortality was slightly lower among Black women than among White women. The death rates diverged sharply after 1980, and this disparity has been persistent.
What triggered the divergence in breast-cancer mortality according to race in the 1980s?
In the 1980s, two medical interventions were widely implemented in the United States for breast-cancer management — mammography screening and adjuvant endocrine therapy — and racial disparities in access to these interventions, as well as in their effects, probably precipitated the divergence in mortality.
Black women are more likely than White women to lack health insurance or to have inadequate coverage, which has limited their access to mammography screening and adversely affected therapeutic decision making. In the 1980s, for example, mammography-screening rates were substantially lower among Black women than among White women, although the rates are now similar.
See the full text of the scientific paper “The Emergence of the Racial Disparity in U.S. Breast-Cancer Mortality” by Ismail Jatoi et al.
Breast Cancer in Hispanic Women
"Story of breast cancer in Hispanic women or Latinas is one that has not been fully told"

Overall, breast cancer rates in Hispanic women are 28 percent lower than in non-Hispanic White women — but that doesn’t give the complete picture. Breast cancer in Latinas and Hispanic women may remain undiagnosed until later stages when it is more difficult and expensive to treat.
That’s one reason Hispanic women and Latinas are about 30 percent more likely to die from their breast cancer than non-Hispanic White women. They are also at higher risk for triple-negative and human epidermal growth factor receptor-positive breast cancers, which are more aggressive than other types of breast cancer.
“Latinas are less likely to seek genetic counseling or testing for breast cancer compared to non-Hispanic White women. They also have lower rates of mammography screening,” says Laura Fejerman, co-director of Latinos United for Cancer Health Advancement or LUCHA at the University of California Davis.
“Low-income Latinas are getting left behind because they are not aware of the role genes play in breast cancer and, if they become aware, often they don’t have access to genetic counseling and testing,” she adds.
Source: “Community health educators help Latinas access breast cancer prevention and treatment” on the UC Davis Health website (May 5, 2022).
State by state breast cancer death rates
Breast cancer death rates in most states are highest for Black women and lowest for Hispanics, Asian Americans, Native Hawaiians, and Pacific Islanders

Source: “Achieving Racial and Ethnic Equity in U.S. Health Care; A Scorecard of State Performance” from The Commonwealth Fund (November 18, 2021)
Breast Cancer Disparities in 10 Major Metropolitan Areas
Susan G. Komen’s initiative Stand for H.E.R., a Health Equity Revolution, aims to reduce breast cancer disparities experienced by Black women starting in the 10 U.S. metropolitan areas where the inequities are greatest.

Susan G. Komen’s initiative Stand for H.E.R., a Health Equity Revolution, aims to reduce breast cancer disparities experienced by Black women starting in the 10 U.S. metropolitan areas where the inequities are greatest.
Read Susan G. Komen’s analysis of the breast cancer disparities in each of these metropolitan areas and what is needed to reduce these disparities.
Closing the Breast Cancer Gap: A Roadmap to Save the Lives of Black Women in America (2021)
