Endometrial cancer disparity facts

B=Black 29.3, NA=Native American 28.1,
W=White 28.0, H=Hispanic 26.0, A=Asian/Pacific Islander 22.6
Source: National Cancer Institute Cancer
Stat Facts: Uterine Cancer

B=Black 9.0, W=White 4.6,
NA=Native American 4.4, H=Hispanic 4.2, A=Asian/Pacific Islander 3.4
Source: National Cancer Institute Cancer
Stat Facts: Uterine Cancer
Incidence
Cancer of the uterine corpus is often referred to as endometrial cancer because more than 90% of cases occur in the endometrium, the lining of the uterine corpus.
Black women. The uterine cancer incidence rate in Black women (28.1 per 100,0000) is similar to that in White women (27.8 per 100,000) without correction for the prevalence of hysterectomy (which eliminates the risk for cervical cancer). A hysterectomy correction results in an 80% increase in the rate for Black women versus a 58% increase for White women, equating to a 15% to 20% higher rate among Black women.
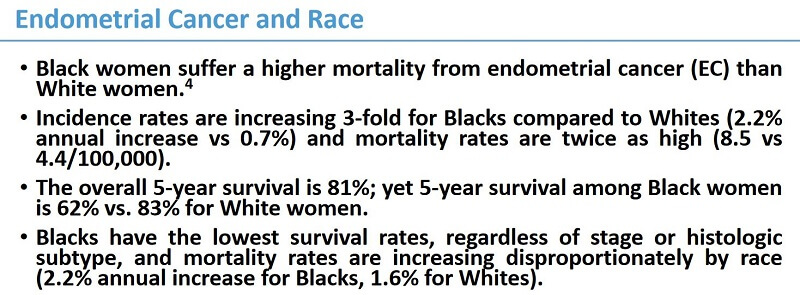
Historically, endometrial cancer incidence rates have been lower in Black than White women but a steeper and earlier increasing trend, beginning in the mid-1990s, has led to the recent convergence of rates. Increased risk may be related to the obesity epidemic, although a subtype that is less strongly associated with obesity appears to be driving the trend. From 2014 to 2018, incidence rates increased by about 2% per year in Black women but appeared to stabilize in White women.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Black women have a higher incidence of uterine cancer than White women. Older studies reported the opposite, but these studies did not account for the higher hysterectomy rate among premenopausal Black women compared with White women, underestimating the true incidence among Black women at risk for uterine cancer. In an analysis of data that adjusted for hysterectomy, the incidence of endometrial cancer among Black women has exceeded that of White women since 2000. The incidence of uterine cancer increased from 1999 to 2015, with larger increases observed among Black women than among White women.
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
Hispanic women. Uterine cancer incidence appears to be lower in Hispanic women than White women. From 1999 to 2015, the incidence increased more significantly for Hispanic women (32%) than for White women (9%). Multiple studies using national databases have shown that Hispanic women were younger at diagnosis.
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
Asian/Pacific Islander women. In 2016, the CDC reported that the uterine cancer incidence rate was lower for Asian/Pacific Islander women than for Black and White women. There was a larger increase in incidence rates from 1999 to 2016 for Asian/Pacific Islander women (38%) than for White women (9%).
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
American Indian/Alaska Native women. American Indian/Alaska Native women appear to have lower uterine cancer incidence rates than other groups. Rates increased 53% from 1999 to 2016.
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
Tumor type
Black women. Black women have a two to four-fold higher incidence of high-risk uterine cancer subtypes, particularly serous carcinoma, carcinosarcoma, and leiomyosarcoma, compared to White women after correcting for hysterectomy and active pregnancy.
Source: Racial disparities in high-risk uterine cancer histologic subtypes: A United States Cancer Statistics study (2021)
Black women are about twice as likely to be diagnosed with uterine clear cell carcinoma as White, American Indian/Alaska Native or Asian/Pacific Islander women. Uterine clear cell carcinoma is a rare aggressive cancer associated with a poor prognosis.
Source: Uterine clear cell carcinoma risk in White versus non-White US subpopulations: does race matter? (2020)
US-born blacks have twice the incidence of endometrial cancer type 2, which is less common but more lethal, as White and Hispanic women and a one-third greater incidence than Caribbean-born Black women.
Source: Endometrial Cancer Type 2 Incidence and Survival Disparities Within Subsets of the US Black Population (2021)
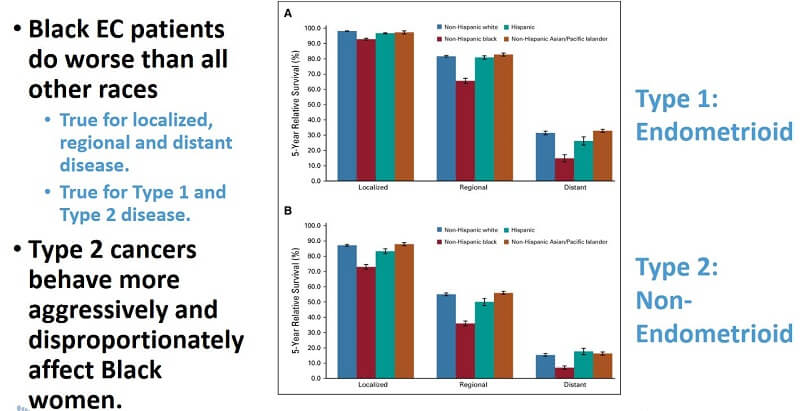
Tumors with aggressive histology accounted for 53% of mortality among Black women, compared with 36% mortality among White women. The disproportionate burden of high-risk histology among Black women contributes to their lower 5-year survival rates. However, even among women with aggressive histologic subtypes, Black women have a significantly higher mortality rate than White women, with Black women having mortality rate ratios ranging from 1.52 to 2.90 for the different high-risk histologic subtypes.
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
Asian women. Vietnamese women are diagnosed with uterine clear cell carcinoma at an average age of 56, significantly younger than other Asian/Pacific Islander women who were diagnosed at average ages of 64 to 72. Uterine clear cell carcinoma is a rare aggressive cancer associated with a poor prognosis.
Source: Uterine clear cell carcinoma risk in White versus non-White US subpopulations: does race matter? (2020)
Diagnosis
Black women. Close to half (44%) of uterine corpus cancers in Black women are diagnosed at an advanced stage or are unstaged (usually advanced) compared to 29% in White women. Survival is lower for Black women for every stage of diagnosis, with the largest difference for regional-stage disease (52% versus 72%.) This may partly reflect a higher prevalence of aggressive uterine cancer subtypes (e.g., uterine serous cancer, uterine carcinosarcoma).
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
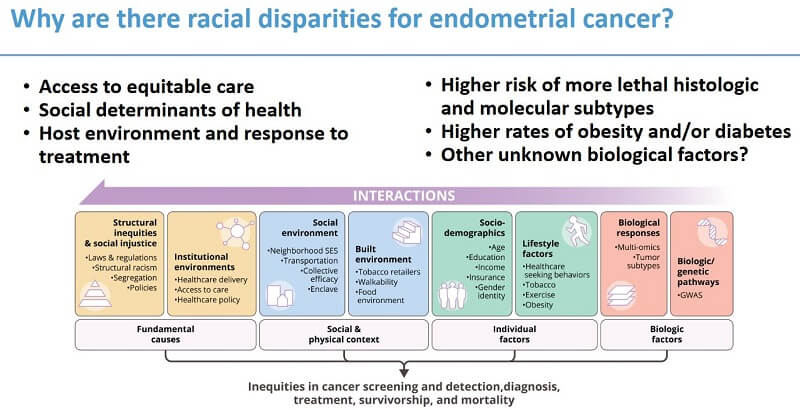
Advanced stage at diagnosis is more common in Black and Hispanic women. Black women are more likely to be diagnosed with nonendometrioid (ie, aggressive) histologies. Black women are less likely to receive guideline-concordant (recommended) diagnostic procedures.
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
Hispanic women. Advanced stage at diagnosis is more common in Black and Hispanic women.
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
Treatment
Black women. Treatment differences accounted for 47% of Black-white differences in cervical cancer mortality and lack of insurance explained 19% of the excess risk for Blacks, according to a recent study. Among early-stage cervical cancer patients, a greater proportion of Black women (17%) failed to receive surgery, which is the standard of care, compared to white (9%) and Hispanic (12%) women.
Source: American Cancer Society. Cancer Facts & Figures for African Americans 2019-2021. Atlanta: American Cancer Society, 2019
Black women are less likely to receive surgery, hysterectomy, or definitive surgical treatment. Minimally invasive surgery is performed less frequently in Black women. Black women are less likely to have lymph node sampling or dissection. Black women are less likely to receive chemotherapy. Black women are less likely to have guideline-compliant (recommended) treatment.
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
Among women with endometrial cancer considered at high risk for recurrence, Black patients were 21% less likely, and Hispanic and Asian
patients were 25% less likely, than White patients to receive recommended adjuvant radiation therapy
Source: Socioeconomic Inequality and Omission of Adjuvant Radiation Therapy in High-Risk, Early-Stage Endometrial Cancer (2021)
Hispanic women. Hispanic women are less likely to receive surgery, hysterectomy, or definitive surgical treatment. Minimally invasive surgery is performed less frequently in Hispanic women. Hispanic women are less likely to have lymph node sampling or dissection. Hispanic women are less likely to have guideline-compliant (recommended) treatment.
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
American Indian/Alaska Native women. American Indian/Alaska Native women are less likely to have guideline-compliant (recommended) treatment.
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
5-year survival
Black women. The Black-White disparity in 5-year relative survival for uterine corpus cancer is among the largest of any cancer: 63% in Black women compared to 84% in White women. Later-stage diagnosis, more aggressive tumors, and lower likelihood of timely optimal treatment contribute to the disparity.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
The most recent statistics from the American Cancer Society reported an absolute difference of 21% in 5-year survival rates, with 63% of Black women surviving compared with 84% of White women. This gap in survival represents the second largest of all racial disparities reported. These disparities in mortality are not new; they have been observed for decades.
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
Mortality
Black women. The uterine corpus cancer death rate in Black women is nearly double that in White women (9.0 versus 4.6 deaths per 100,000, respectively, likely due to unequal access to high-quality treatment. From 2010 to 2019, the death rate increased by about 2% per year in Black women, similar to increases in White women.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Black women with advanced endometrial cancer survived a median of 29 months after diagnosis vs 56 months for White women, in a study of US patients between 2013 and 2020.
Source: Real-world outcomes in patients with advanced endometrial cancer: A retrospective cohort study of US electronic health records (Supplementary data) (2022)
In 2016, deaths from uterine cancer among Black women were nearly twice as frequent as any other racial or ethnic group. Survival for Black women with uterine cancer was lower than for White women for every stage, grade, and histologic subtype and for every age group.
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
Black women with endometrial cancer had significantly shorter overall survival than White women in an equal access U.S. military healthcare system, despite accounting for traditional clinical and pathological characteristics, suggesting that factors other than access to care may be related to this racial disparity.
Source: Racial disparities in survival among women with endometrial cancer in an equal access system (2021)
Hispanic women. Most studies have concluded that Hispanic women have similar or improved survival compared with White women after controlling for tumor characteristics, age and other sociodemographic factors, cancer stage, and treatment.
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
Asian/Pacific Islander women. In analyses of data from 1988 to 2009 and from 2000 to 2011, Asian women had better overall and uterine cancer-specific mortality than non-Hispanic White women.
Source: “Health Disparities in Uterine Cancer: Report from the Uterine Cancer Evidence Review Conference” (April 2022)
Source: Racial Disparities in Endometrial Cancer: Molecular Studies of Black Women with Endometrial Cancer by Victoria Bae-Jump, MD, PhD (2022)
Carol L. Brown, MD
"We have an epidemic of endometrial cancer in Black women in this country"
“We have an epidemic of endometrial cancer in this country and it is disproportionately affecting Black women.
“The number of endometrial cancer cases has increased by 57 percent in the last 10 years. This is not seen in any other GYN cancer,” says Carol L. Brown, MD, of the Memorial Sloan Kettering Cancer Center in New York
For Black women, the increase in both the number of cases and the number of deaths per 100,000 women is rising and it’s rising at a much higher rate than it is for any other racial or ethnic group.”
A 2-minute video, part of a presentation to the Black Health Matters Winter Summit in February 2021.
"Black women are significantly more impacted by high-risk endometrial cancers"

“When you look at serous carcinomas (which accounts for most of the deaths from this cancer), they’re increasing over 6% every single year for Black women for almost the last 20 years, says Cortney Eakin, MD, of the University of California, Los Angeles.
That’s a lot! If that trend continues over the next 10 years, when a Black woman gets diagnosed with uterine cancer, she’s going to be three times as likely to get a high-risk cancer compared with a low-risk one.
Uterine Cancer Is on the Rise, Especially Among Black Women
Cancer of the uterus, also called endometrial cancer, is increasing so rapidly that it is expected to displace colorectal cancer by 2040 as the third most common cancer among women, and the fourth-leading cause of women’s cancer deaths.
The mortality rate has been increasing by almost 2 percent a year overall, with even sharper spikes among Asian, Hispanic and Black women.
Uterine cancer was long believed to be less common among Black women. But newer studies have confirmed that it is not only more likely to strike Black women, but also more likely to be deadly.
Black women die of uterine cancer at twice the rate of white women and are also more likely to develop a form called non-endometrioid uterine cancer, which is more aggressive.
Source: “Uterine Cancer Is on the Rise, Especially Among Black Women” by Roni Caryn Rabin on the New York Times website (June 17, 2022)
Endometrial cancer provides a compelling example of medical racism hiding in plain sight
 “We know Black women have more fibroids, and we know they are more likely to have the kinds of endometrial cancer that do not always cause thickness measured on ultrasound,” says Kemi M. Doll, MD, of the University of Washington School of Medicine . “So how did we come up with a diagnostic strategy based on a test—transvaginal ultrasound—that’s so differentially impactful?” she asks.
“We know Black women have more fibroids, and we know they are more likely to have the kinds of endometrial cancer that do not always cause thickness measured on ultrasound,” says Kemi M. Doll, MD, of the University of Washington School of Medicine . “So how did we come up with a diagnostic strategy based on a test—transvaginal ultrasound—that’s so differentially impactful?” she asks.
“Naturally, as researchers, we might look at who’s doing the worst, who’s dying from this disease, then figure out the guidelines. But that is not what happened here.”
“An effect of systemic racism is seen in the fact that our goal was avoiding biopsies in the population of convenience, the majority, rather than the group most at risk.”
Similarly, the limitations of the data are difficult to dispute. “When we demonstrate that the guidelines are based on studies out of Scandinavia, Italy, and Hong Kong and largely exclude or fail to report on women with fibroids, it’s easy to see that’s not objective,” Dr. Doll says.
Source: “What the Science of Uterine Cancer Reveals about Medical Racism” on the American College of Obstetricians and Gynecologists website (2022)
