Lung cancer clinical trials
Saved by a lung cancer clinical trial
Not only did a clinical trial save her life, but her family came back asking about clinical trials for others
I had a patient in my clinic in Mississippi with widespread lung cancer, says lung cancer specialist Raymond U. Osarogiagbon, MD, Chief Scientist for Baptist Memorial Health Care in Memphis, Tennessee. “I talked to her about the clinical trial we had and she was interested, but she needed to come back with her family.”
 “There were — I kid you not — 30 people that came with her and I sat them down and explained why the clinical trial was a good idea for her.”
“There were — I kid you not — 30 people that came with her and I sat them down and explained why the clinical trial was a good idea for her.”
“It was time well spent. Because not only did she get on the clinical trial. Not only did she stay on the clinical trial on a treatment that turned out to be the new standard treatment for this terrible cancer she had. But since that time, she and her family have come back with not only gratitude, but also when others have been diagnosed with the cancer, they have come back asking if there was a clinical trial!”
A wonderful 2-minute video from the National Cancer Institute.

"I am on my second life on this earth. This is what science has done for me."
“When I was given my diagnosis of advanced lung cancer, they told me I had less than six months to live and to get all my affairs in place,” Barry Nelson remembers. “I was a smoker for 37 years. My mother, she died from cancer. My mother’s sisters and her mother died from cancer. I really was quite arrogant and prideful and not taking the time to realize what I was doing to myself.”
“I prayed to God and He said, you’re going to die but you’re not right now. I went through a number of different treatments, not getting the results they were looking for.”
Having exhausted his treatment options, “I was one of the first lung cancer patients to participate in a clinical trial with immunotherapy. Immediately when I had my first infusion, it was just a whole new feeling. And I knew that something was different.”
“As a cancer survivor for the last 10 years, I’m not on any type of medication or treatment and I am on my second life here on this earth. I hope that I’m a better person. This is what science has done for me.”
A 4-minute video from the National Cancer Institute.
"We are dealt a deck of cards in life. And it is about how to play our cards that matters.”

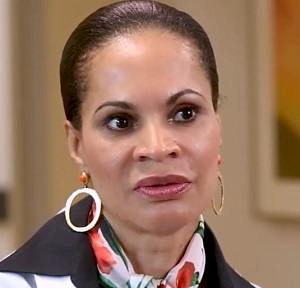
At the start of the COVID-19 pandemic, Sheena began experiencing terrible ear pain. Doctors couldn’t figure out what was causing her pain, until her primary care physician did a chest X-ray and noticed a mass in her lung.
She was diagnosed with advanced lung cancer, which came as a shock since she had no known risk factors. Biomarker testing showed that it was EGFR-positive non-small cell lung cancer. Her oncologist suggested a clinical trial might be the most appropriate treatment option for her at the time and she agreed to participate.
Sheena now takes a pill once a day which keeps her cancer under control. The clinical trial is highly monitored, and Sheena is in close contact with her physicians so they can address any side effects that might occur.
She is passionate about sharing her experience with other Black lung disease patients to raise awareness of the importance of self-advocacy, education and making informed care choices.
“As my father used to say, we are dealt a deck of cards in life. And it is about how to play our cards that matters. I don’t want anyone facing lung disease to miss out on receiving the best care for them, which may be a clinical trial,” says Sheena.
Source: “The Importance of Representation in Lung Cancer Clinical Trials” by Carly Ornstein on the American Lung Association website (2022)
What are clinical trials and why join one?
Cancer clinical trials allow researchers to study innovative and potentially life-saving new treatments. The goal is to find treatments that are better than what’s currently available.
Placebos are rarely used in cancer treatment clinical trials. If participants don’t receive the study medication, they are always given the best available treatment for their particular cancer. This helps the researchers determine whether the study medication is better than the standard treatment.
A 2-minute video from Stand Up to Cancer
Reason one. You have a chance to receive treatment based on the latest research that is not yet available to others. Clinical trials are based on the best knowledge available for your kind of cancer.
Reason two. You’ll get high-quality care and be carefully monitored throughout the study.
Reason three. You add to the world’s knowledge about cancer and help to improve cancer care for future generations.
A 2-minute video from the National Cancer Institute
“There are some well founded reasons why there is mistrust in research because of well documented historical abuses,” says Lannis Hall, M.D.
“I have told patients for years, if they want to ensure the absolute best care, then they want to request participation on a clinical study. It is because the safeguards in clinical trials are multilayered.”
“Clinical trials test new drugs or new regimens or different ways of treating cancer against the current standard to see if the new interventions would be better than what we currently have,” says Foluso Bisi Ademuyiwa, M.D.
A 5-minute promotional video for the Siteman Cancer Center in St. Louis, one of 71 National Cancer Institute-Designated Cancer Centers in the United States.
“We know that patients who are enrolled on studies today typically have a better outcome than those who are not enrolled in studies. They’re going to be getting nothing less than the standard of care,” says Jeff Michalski, M.D.
“And often the oversight and quality assurance that goes along with that leads to a better outcome.”
"It really is the clinical trial that determines how we take care of lung cancer patients"
“We do clinical trials in order to understand processes that are involved in lung cancer, whether that’s the treatments that are effective or whether they’re safe,” says Manish Patel, D.O., and oncologist and researcher at the University of Minnesota.
“It really is the clinical trial that determines how we take care of patients. All of these clinical trials are involved in developing the best therapy for patients with lung cancer.
Without clinical trials, we really don’t know what the best treatments are or how to choose the treatment for a patient with with lung cancer.
So they’re incredibly important.”
A 1-minute video from You and Lung Cancer
Clinical trials can help improve survival and quality of life for you and others with lung cancer
Researchers need different people to take part in different clinical trials. For example, a particular trial may need volunteers with a certain type or stage of lung cancer, or of a certain age, sex or ethnicity.
The benefit of taking part in a clinical trial is that it allows you to try a drug treatment or procedure that is not yet available to the public. The risk is that you may experience unwanted side effects. The trial may benefit your health or it may not, but the knowledge that researchers gain will benefit people in the future.
Ask your doctor about joining a clinical trial. You can ask any time before or during treatment. You can leave a clinical trial at any time and you will still receive treatment for your lung cancer unless you want to stop that.
A 6-minute video from You and Lung Cancer and developed by A Breath of Hope Lung Foundation and Mechanisms in Medicine Inc. with support from pharmaceutical companies.

W=White 85.6%, B=Black 8.3%, A=Asian 4.8%, H=Hispanic 1.1%, AI=American Indian and Alaskan Native 0.2%
Among 93 clinical trials for breast, colorectal, lung, and prostate cancers from 2004 to 2017, lung cancer studies had the highest proportion of White and Asian participants and the lowest proportion of Black, Hispanic, and American Indian/Alaskan Native participants.
Source: Racial and Ethnic Disparities Among Participants in Precision Oncology Clinical Studies (2021)
Precision oncology clinical trials test potential treatments targeted to specific genetic mutations that may be driving tumor growth. In this study of 26 lung cancer trials that were conducted between 2004 and 2017, researchers calculated for racial/ethnic groups the ratio of their participation in the trials to their prevalence of lung cancer in the population.
 Black representation in the trials was 68 percent lower and Hispanic representation 69 per cent lower than their share of lung cancer in the U.S. population. On the other hand, White representation was 40 percent higher and Asian representation nearly 300% percent higher than it should have been if it had matched their share of lung cancer.
Black representation in the trials was 68 percent lower and Hispanic representation 69 per cent lower than their share of lung cancer in the U.S. population. On the other hand, White representation was 40 percent higher and Asian representation nearly 300% percent higher than it should have been if it had matched their share of lung cancer.
“Current personalized treatments that are broadly generalized to all individuals based on the presence or absence of a biomarker without fully studying the implications of such treatment in racial and ethnic minority populations may not be appropriate,” Sophia C Kamran, M.D., (left) of the Massachusetts General Hospital and her colleagues wrote.
Source: “Racial and Ethnic Disparities Among Participants in Precision Oncology Clinical Studies” (2021).
The disparities in clinical trials significantly affect the efficacy of treatment for under-represented groups. This impact will only increase as the trend of personalized medicine continues and treatments like immunotherapy are explicitly tailored to one’s genes. Without sufficient data regarding a patient group, doctors have limited ability to predict how they may respond to treatment.
For example, a 2017 study found that some African Americans have lung tumors with a different gene expression than those found in white patients. This could impact the efficacy of specific therapies.
In the U.S., patients who enroll in cancer treatment trials tend to be younger, male, and white. This lack of diversity in clinical trials can lead to a cycle where new treatments are most effective for the most represented group. The results are not generalizable or misapplied to certain populations and perpetuate health disparities in the lung cancer continuum.
Source: “Lack of Diversity in Clinical Trials: A Patient’s Guide” (Lung Cancer Foundation of America)
How else will we know that a new treatment works as well for all races, ethnicities, ages and genders?

Clinical trials provide individuals with cancer the opportunity to participate in groundbreaking research that may bring about new treatments that improve quality of life, extend survival, and even prove lifesaving. Research and results that come from clinical trials also shed light on the side effects that participants experience during the study.
If people from all groups are not represented in clinical trials, we will not know if a new cancer treatment works as well for all ages, genders, races, and ethnic groups. We also will not know if some groups are more likely than other groups to develop side effects.
If all groups are not represented in clinical trials, they will not have the chance to benefit equally from the newest treatments. This can widen the differences we see in cancer outcomes in the U.S.
Source: “The Importance of Diversity in Clinical Trials,” an 8-page brochure from The Cancer Support Community (2021)
Critical information is gained only by participating in clinical trials
“I always try to explain to my patients the importance for minorities to participate in the clinical trials so that we’re represented in data analysis,” says Patricia Robinson, M.D., a cancer physician-researcher and Associate Dean in the Stritch School of Medicine at Loyola University, Maywood, Illinois.
“We don’t all metabolize drugs the same way and I think it’s important for people to recognize, within their patient population based upon genetics, what the potential benefit may be as well as the potential toxicities. If you are a slow metabolizer or quick metabolizer, that information is only gained by participating in clinical trials and having the data analyzed.”
A 2-minute video from the Cancer Support Community.
“Clinical trials play a big role in our medical decision making. Simply put, you need to be represented for us to make a good decision based on your particular cancer and how it works in your body,” says Janine Harewood, M.D., an oncologist in Ft. Myers, Florida.
Some reasons why you should participate in clinical trials: you get first access to drugs which are not available in the general population as yet; you’re more likely to get frequent health checkups just because you need to be closely monitored; and it’s an opportunity to make a difference and help other patients gain from the information that we learn.”
“But it does come with risks. It’s a clinical trial because we don’t know everything. We’re trying to assess how the drug works, if it does work or if there any side effects.”
“The most common fear I hear from patients is that they won’t get the treatment when they’re on trial. Clinical trials today are not like they were. Now when clinical trials are designed, there’s the trial drug and then there’s the standard of care, not a placebo.”
“Clinical trials are always an option. Even if you’re not confident right now about going into a clinical trial and you’re comfortable with your treatment, there’s no harm in seeing what your options are.”
“I encourage you in the same way I would encourage my family. Please open yourself to the idea of a clinical trial and at least make sure that you get all the information so that you can make an informed decision.”
A 4-minute video from You and Lung Cancer.
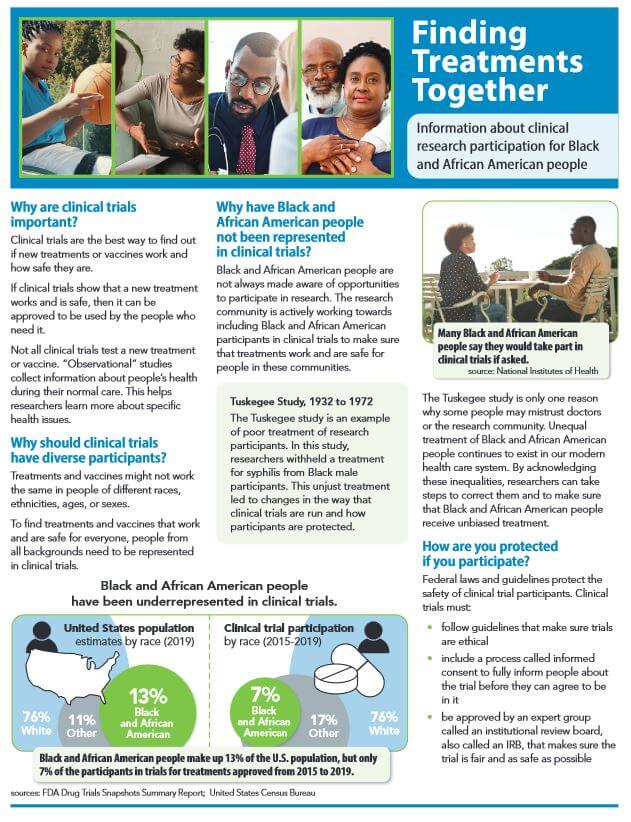
Source: Center for Information and Study on Clinical Research Participation, Inc.(CISCRP), a non-profit 501(c)(3) organization advocating for clinical research education.
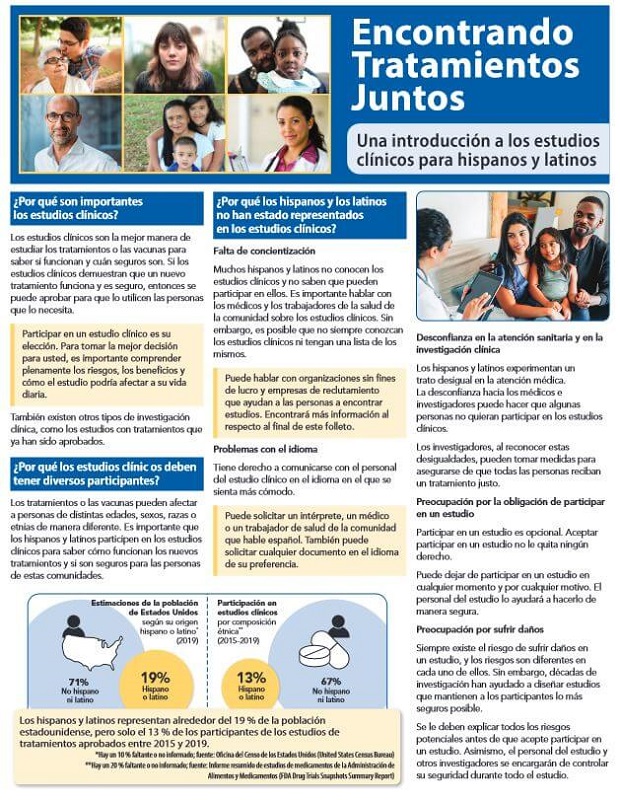
Source: Center for Information and Study on Clinical Research Participation, Inc.(CISCRP), a non-profit 501(c)(3) organization advocating for clinical research education.

A free, over-the-phone service that helps Black or African American (AA) cancer patients learn more about clinical trials.
The Peer Clinical Trials Support Program matches interested patients with a peer — a Black or African American cancer patient or survivor with experience participating in a cancer clinical trial. Patients have the opportunity to discuss their fears, questions, and concerns with a knowledgeable and empathetic guide, and hear from someone of a similar background who has “been there, done that.”
Source: Cancer Support Community
National Cancer Institute
 If you are thinking about taking part in a clinical trial, be sure to ask your doctor, “Is there a clinical trial that I can join?” If your doctor offers you a trial, here are some questions you may want to ask, such as:
If you are thinking about taking part in a clinical trial, be sure to ask your doctor, “Is there a clinical trial that I can join?” If your doctor offers you a trial, here are some questions you may want to ask, such as:
More at: “Questions to Ask Your Doctor about Treatment Clinical Trials” (National Cancer Institute)
American Cancer Society

- What phase is this clinical trial in?
- Why is this study being done?
- How long do I have to make this decision?
- What’s likely to happen if I decide to take part or not take part in the clinical trial?
- Will the researchers work with my cancer doctor? Who will be in charge of my care?
- Who will I get in touch with if I have problems, questions, or concerns?
- What are my other options (standard treatments, other clinical trials)? What are the pros and cons of each?
- How much do you know about this treatment? About clinical trials in general?
- What were the results in past studies of this treatment? How likely are they to apply to me?
- Is there anything else I can read about this clinical trial?
- What kinds of treatments and tests would I need to have? How often are they done?
- Would I need to plan on extra time or travel?
And more questions at “Deciding Whether to Be Part of a Clinical Trial” by the American Cancer Society (2022)
Steps to Find a Clinical Trial
Learn how to find the right clinical trial for you with the National Cancer Institute’s six-step guide:
Step 1: Gather Details about Your Cancer
Step 2: Find Clinical Trials
Step 3: Take a Closer Look at the Trials that Interest You
Step 4: Contact the Team Running the Trial
Step 5: Ask Questions
Step 6: Make an Appointment
A 2-minute video from the National Cancer Institute
Help finding lung cancer clinical trials from government agencies
ClinicalTrials.gov is a database of privately and publicly funded clinical studies conducted in all 50 states and in 221 countries.
The website provides current information about clinical research studies for patients, their families and caregivers, health care professionals, and the public.
Each study record includes a summary of the study protocol, including the purpose, recruitment status, and eligibility criteria. Study locations and specific contact information are listed to assist with enrollment.
Information on ClinicalTrials.gov is provided and updated by the organizations and people that sponsor and carry out the studies. Listing a study does not mean it has been evaluated by the U.S. Federal Government.
Clinicaltrials.gov is a free service of the National Institutes of Health (NIH) and is maintained by the National Library of Medicine (NLM).
For more information about using the database, visit clinicaltrials.gov

“If you decide to look for trials on your own, learn how to find the right clinical trial for you with the National Cancer Institute’s six-step guide:
- Step 1: Gather details about your cancer
- Step 2: Find clinical trials
- Step 3: Take a closer look at the trials that interest you
- Step 4: Contact the team running the trial
- Step 5: Ask questions
- Step 6: Make an appointment
The NCI’s Cancer Information Service can also provide a tailored clinical trials search that you can discuss with your doctor. To reach them call 1-800-4-CANCER (1-800-422-6237) and select option 2. This is a free service. Keep in mind that the search results do not replace advice from your doctor.
Source: National Cancer Institute (2022)
Help from non-profit 501(c)3 charitable organizations

Our Cancer Immunotherapy Clinical Trial Finder will aid you in finding your answer to cancer. Understand the basics of cancer clinical trials, why clinical trials are so critical to our work, what things to consider about enrolling, and how to assist patients in finding clinical trials for which they may be eligible.
Source: Cancer Research Institute, a 501(c)3 charitable organization.
Standup to Cancer
Source: Stand up to Cancer, a division of the Entertainment Industry Foundation (EIF), a 501(c)(3) charitable organization.
If you are a cancer patient who needs help identifying clinical trial options or needs financial assistance to attend a clinical trial, we’d like to hear from you. Our Patient Navigator can help you find the right clinical trial. We can also help you with the costs associated with participating in a clinical trial, including transportation and lodging.
For more information, email Lazarex or to speak with a Lazarex representative, call 925.820.4517.
Source: Lazarex Cancer Foundation, a 501(c)3 charitable organization.


Finding the right trial can be overwhelming. Search Clinical Trials is a free service designed to help people find clinical trials that are relevant to their medical and healthcare needs.
The CISCRP team will work with you to understand your options and help you find local clinical trials in your community, or as far as you would be comfortable traveling.
Source: Center for Information and Study on Clinical Research Participation, Inc.(CISCRP), a non-profit 501(c)(3) organization advocating for clinical research education.
Help from private companies
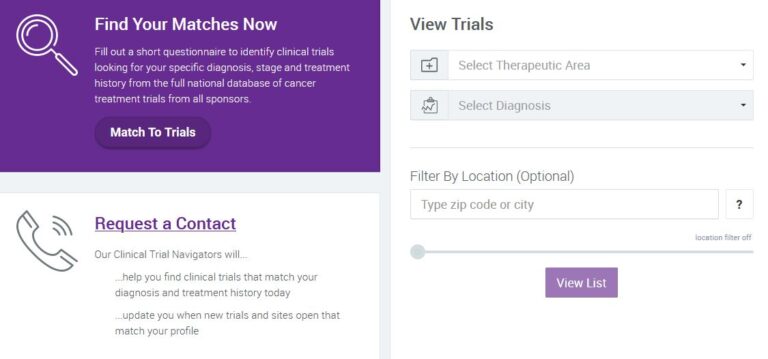
For over a decade, EmergingMed’s clinical navigators have facilitated clinical trial searches for nearly 500,000 patients. Request a Contact today to learn how we are able to help.
Source: EmergingMed

“As a digital patient engagement company, Antidote’s focus is on connecting patients to clinical trials — that’s why we have a moral imperative to support diversity, equity, and inclusion (DEI) initiatives that ensure clinical trial populations reflect those of the real world.”
Source: Antidote
“Our site has a comprehensive listing of all trials in the United States and is categorized to help you find it quick. ClinicalTrialsGPS has information on trials from all the leading pharmaceutical companies, academic institutions and trials ranging from Cancer to Diabetes and Vaccines to Osteoarthritis.”
“Our goal is to provide you with the most comprehensive, up to date information about ongoing clinical studies as well as a quick and easy way to participate. “
Source: Clinical Trials GPS

Search and browse to find a trial relevant to you. Read the trial details on eligibility, location and participation. You can also register to be notified when a trial you’re searching for begins. Find a trial near you.
Source: Center Watch