Endometrial Cancer Disparities
- diagnosed at a later stage of endometrial cancer
- more likely to have aggressive tumors
- less likely to receive optimal surgical treatment
- about twice as likely to die of endometrial cancer
News






Black patients wait longer for endometrial cancer testing and diagnosis



Black and Hispanic women missing from endometrial cancer clinical trials



Data

B=Black 29.3, NA=Native American 28.1,
W=White 28.0, H=Hispanic 26.0, A=Asian/Pacific Islander 22.6
Source: National Cancer Institute Cancer
Stat Facts: Uterine Cancer

B=Black 9.0, W=White 4.6,
NA=Native American 4.4, H=Hispanic 4.2, A=Asian/Pacific Islander 3.4
Source: National Cancer Institute Cancer
Stat Facts: Uterine Cancer
Women Diagnosed with Endometrial Cancer
Gwen Ifill

Journalist Gwen Ifill died of breast and endometrial cancer in 2016 at age 61, surrounded by family and friends. She had been suffering from endometrial cancer for less than a year.
Ifill was the first African-American woman to host a nationally televised U.S. public affairs program and moderated the 2004 and 2008 vice-presidential debates.
Rocio Durcal
Spanish singer and actress Rocío Dúrcal, beloved singer in Latin America, died in 2006 at age 61 from endometrial (uterine) cancer.
She was diagnosed in 2001. Three years later, her doctors discovered a malignant lesion in her lungs, which was treated with chemotherapy. The cancer later metastasized to her brain and she died in her home in Madrid.
Ann Dunham

Ann Dunham, mother of Barack Obama, died from uterine cancer at age 52 in late 1995.
Her cancer was misdiagnosed as indigestion in Indonesia and had spread to her ovaries by the time she returned to the States earlier that year.
Dunham earned a doctorate in anthropology and spent most of her adult life overseas, particularly in Indonesia.
Nefa-Tari Moore

In August of 2013, 33-year-old Nefa-Tari Moore, a licensed practical nurse (LPN) in Brooklyn, New York, started experiencing heavy vaginal bleeding and lower back pain. She didn’t think much of it at first—until one day in November when her pain became so severe she rushed to a hospital emergency room.
There she was told told that the bleeding might just be a change of menstrual cycles, or her being stressed, or “that it was all in my head,” Moore says. “They wanted to give me ibuprofen and recommended that I go home and rest.”
But Moore insisted on staying for further observation until the ER staff set her up with an OB/GYN referral, which ultimately led to her diagnosis of endometrial cancer.
She now works with the Spot Her campaign to raise awareness about endometrial cancer and to empower women “to be their own best advocates for their health.”
Linda Collins

Linda Collins had been in menopause for almost a decade when she started bleeding again. The bleeding was light — occasional spotting, really — and she barely gave it a passing thought.
When she finally went in for a checkup, her doctor refused to let her leave until she underwent a biopsy. Within days, Ms. Collins learned she had cancer of the uterus — and an especially aggressive form of it.
“I had no pain, no other symptoms, and I didn’t think seriously about it,” said Ms. Collins, 64, a retiree in New York City. “That was a mistake.”
Collins underwent a hysterectomy and radiation therapy and now goes out of her way to tell friends and acquaintances to immediately talk to their doctors about unusual bleeding or other symptoms like pain, bloating or sudden weight loss.
“I tell them, ‘Don’t wait, don’t wait. If it doesn’t feel right, if you don’t think it should be happening — check it out,’” Ms. Collins said. “I should have looked into it sooner.”
Source: “Uterine Cancer Is on the Rise, Especially Among Black Women”
“Endometrial cancer is actually the most common GYN cancer in the United States. It’s four times more common than cervical cancer, it’s twice as common as ovarian cancer. As a GYN oncologist, we see women with endometrial cancer every day and often we’ll hear that women had never heard of it before they were diagnosed.”
Kemi Doll, MD, of the University of Washington

Endometrial Cancer Disparities
Incidence
Cancer of the uterine corpus is often referred to as endometrial cancer because more than 90% of cases occur in the endometrium, the lining of the uterine corpus.
Black women. The uterine cancer incidence rate in Black women (28.1 per 100,0000) is similar to that in White women (27.8 per 100,000) without correction for the prevalence of hysterectomy (which eliminates the risk for cervical cancer). A hysterectomy correction results in an 80% increase in the rate for Black women versus a 58% increase for White women, equating to a 15% to 20% higher rate among Black women.
Historically, endometrial cancer incidence rates have been lower in Black then White women but a steeper and earlier increasing trend, beginning in the mid-1990s, has led to the recent convergence of rates. Increased risk may be related to the obesity epidemic, although a subtype that is less strongly associated with obesity appears to be driving the trend. From 2014 to 2018, incidence rates increased by about 2% per year in Black women but appeared to stabilize in White women.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Tumor type
Black women. Black women have a two to four-fold higher incidence of high-risk uterine cancer subtypes, particularly serous carcinoma, carcinosarcoma, and leiomyosarcoma, compared to White women after correcting for hysterectomy and active pregnancy.
Source: Racial disparities in high-risk uterine cancer histologic subtypes: A United States Cancer Statistics study (2021)
Black women are about twice as likely to be diagnosed with uterine clear cell carcinoma as White, American Indian/Alaska Native or Asian/Pacific Islander women. Uterine clear cell carcinoma is a rare aggressive cancer associated with a poor prognosis.
Source: Uterine clear cell carcinoma risk in White versus non-White US subpopulations: does race matter? (2020)
US-born blacks have twice the incidence of endometrial cancer type 2, which is less common but more lethal, as White and Hispanic women and a one-third greater incidence than Caribbean-born Black women.
Source: Endometrial Cancer Type 2 Incidence and Survival Disparities Within Subsets of the US Black Population (2021)
Vietnamese women are diagnosed with uterine clear cell carcinoma at an average age of 56, significantly younger than other Asian/Pacific Islander women who were diagnosed at average ages of 64 to 72. Uterine clear cell carcinoma is a rare aggressive cancer associated with a poor prognosis.
Source: Uterine clear cell carcinoma risk in White versus non-White US subpopulations: does race matter? (2020)
Stage at diagnosis
Black women. Close to half (44%) of uterine corpus cancers in Black women are diagnosed at an advanced stage or are unstaged (usually advanced) compared to 29% in White women. Survival is lower for Black women for every stage of diagnosis, with the largest difference for regional-stage disease (52% versus 72%.) This may partly reflect a higher prevalence of aggressive uterine cancer subtypes (e.g., uterine serous cancer, uterine carcinosarcoma).
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Treatment
Black women. Treatment differences accounted for 47% of Black-white differences in cervical cancer mortality and lack of insurance explained 19% of the excess risk for Blacks, according to a recent study. Among early-stage cervical cancer patients, a greater proportion of Black women (17%) failed to receive surgery, which is the standard of care, compared to white (9%) and Hispanic (12%) women.
Source: American Cancer Society. Cancer Facts & Figures for African Americans 2019-2021. Atlanta: American Cancer Society, 2019
5-year survival
Black women. The Black-White disparity in 5-year relative survival for uterine corpus cancer is among the largest of any cancer: 63% in Black women compared to 84% in White women. Later-stage diagnosis, more aggressive tumors, and lower likelihood of timely optimal treatment contribute to the disparity.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Mortality
Black women. The uterine corpus cancer death rate in Black women is nearly double that in White women (9.0 versus 4.6 deaths per 100,000, respectively, likely due to unequal access to high-quality treatment. From 2010 to 2019, the death rate increased by about 2% per year in Black women, similar to increases in White women.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Black women with advanced endometrial cancer survived a median of 29 months after diagnosis vs 56 months for White women, in a study of US patients between 2013 and 2020.
Source: Real-world outcomes in patients with advanced endometrial cancer: A retrospective cohort study of US electronic health records (Supplementary data) (2022)
Carol L. Brown, MD
"We have an epidemic of endometrial cancer in Black women in this country"
“We have an epidemic of endometrial cancer in this country and it is disproportionately affecting Black women.
“The number of endometrial cancer cases has increased by 57 percent in the last 10 years. This is not seen in any other GYN cancer,” says Carol L. Brown, MD, of the Memorial Sloan Kettering Cancer Center in New York
For Black women, the increase in both the number of cases and the number of deaths per 100,000 women is rising and it’s rising at a much higher rate than it is for any other racial or ethnic group.”
A 2-minute video, part of a presentation to the Black Health Matters Winter Summit in February 2021.
"Black women are significantly more impacted by high-risk endometrial cancers"

“When you look at serous carcinomas (which accounts for most of the deaths from this cancer), they’re increasing over 6% every single year for Black women for almost the last 20 years, says Cortney Eakin, MD, of the University of California, Los Angeles.
That’s a lot! If that trend continues over the next 10 years, when a Black woman gets diagnosed with uterine cancer, she’s going to be three times as likely to get a high-risk cancer compared with a low-risk one.
Uterine Cancer Is on the Rise, Especially Among Black Women
Cancer of the uterus, also called endometrial cancer, is increasing so rapidly that it is expected to displace colorectal cancer by 2040 as the third most common cancer among women, and the fourth-leading cause of women’s cancer deaths.
The mortality rate has been increasing by almost 2 percent a year overall, with even sharper spikes among Asian, Hispanic and Black women.
Uterine cancer was long believed to be less common among Black women. But newer studies have confirmed that it is not only more likely to strike Black women, but also more likely to be deadly.
Black women die of uterine cancer at twice the rate of white women and are also more likely to develop a form called non-endometrioid uterine cancer, which is more aggressive.
Source: “Uterine Cancer Is on the Rise, Especially Among Black Women” by Roni Caryn Rabin on the New York Times website (June 17, 2022)
Voices and Campaigns
Kemi Doll, MD
“I co-founded ECANA, which is the Endometrial Cancer Action Network for African Americans,” says says Kemi Doll, MD, of the University of Washington. “And part of the reason was that with endometrial cancer, Black women have a 90 percent higher mortality rate than all other groups of women in the United States. This is a larger difference in racial disparity than we see in breast cancer.”
“Part of it is definitely the fact that people don’t know about this cancer. Another reason is that the quality of our healthcare system isn’t really the same for Black women as it is for everybody else, especially when it comes to their reproductive healthcare.”
“We don’t know why but Black women do have a higher likelihood of having a more aggressive kind of endometrial cancer. In fact, that’s the reason why Black women should have the most awareness and be ready to go in terms of symptoms and getting evaluated.”
A 3-minute video from the University of Washington.
More information at Endometrial Cancer Action Network for African Americans
Spot Her
Uterine cancer is the 4th most frequently diagnosed cancer for women in the U.S. In 2020, uterine cancer resulted in about 65,000 new cases and 12,500 deaths—and these rates are on the rise.
Spot Her is an initiative to help end the silence around endometrial cancer. We aim to embrace the power of every woman’s voice to take a stand on this important women’s health issue. Together we can educate, support, and build strength through community.
Women with endometrial cancer have reported that their symptoms were often stigmatized and dismissed. By talking about these “below the belt” symptoms, we can empower others to spot the signs early and take action, when it may be more treatable.
Increasing awareness about the potential signs of endometrial cancer is important for Black women, as only 53% of Black women with the condition receive an early diagnosis. A delay in diagnosis could make the disease more difficult to treat.
About Endometrial Cancer
If you have endometrial cancer or are close to someone who does, knowing what to expect can help you cope. Here you can find out all about endometrial cancer, including risk factors, symptoms, how it’s found, and how it’s treated.
Uterine (endometrial) cancer is the most common gynecologic cancer in the United States. Learn how to lower your risk and about the symptoms, risk factors, and treatment for uterine cancer.
Endometrial cancer can often be cured. Explore the links here to learn more about uterine cancer prevention, screening, treatment, statistics, research, and clinical trials.
Signs and Symptoms of Endometrial Cancer
“The most common symptoms of endometrial cancer are vaginal bleeding, vaginal spotting, or any kind of an abnormal vaginal discharge,” says Ursula A. Matulonis, MD, cancer physician at the Dana-Farber and Brigham and Women’s Cancer Center in Boston.
“For a woman who is currently menstruating, if she notices that her periods become much heavier or she’s having bleeding in between periods, that should definitely be brought to the attention of a physician. Other signs and symptoms could include pelvic pain, bloating, difficulty with urination, abnormal urination.”
A 2-minute video from the Dana-Farber Cancer Institute.
How is Endometrial Cancer Diagnosed?
“That’s a good question,” says Jennifer Gilby MD, of Women’s Care Florida.
“Typically, an ultrasound will measure the endometrial cell lining. If you’re menopausal and your lining is greater than 4 millimeters, an endometrial biopsy should be performed.
If you’re having abnormal bleeding and in menopause, you should have your healthcare provider perform an endometrial biopsy.
A 2-minute video from Women’s Care Florida, a specialty women’s health physician group.
About Endometrial Cancer from the National Cancer Institute
Endometrial cancer is most often diagnosed in women aged 55 to 64.
White women have the highest incidence rate, but the death rate for Black women is much higher than all other groups. Lack of medical coverage and unequal access to cancer treatment may contribute to this disparity.
This video Includes information about symptoms and what increases or decreases the risk of developing endometrial cancer.
A 3-minute video from the National Cancer Institute.
Signs and Symptoms of Endometrial (Uterine) and Other Gynecologic Cancers
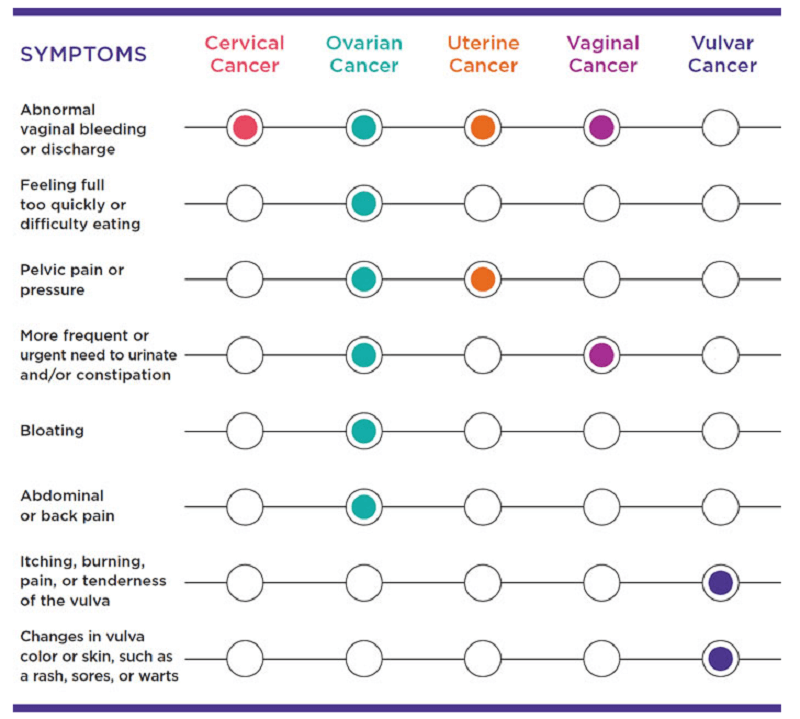
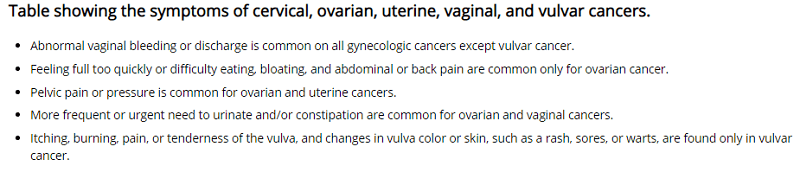
Source: Centers for Disease Control and Prevention (CDC)
“The really important thing to know about bleeding is that it doesn’t have to be a lot of bleeding. It doesn’t have to be something heavy or even painful. A few drops of blood is enough to prompt an evaluation.”
Kemi Doll, MD, of the University of Washington

"Do not wait, do not hesitate"
“I am a survivor of endometrial cancer. Early detection saved my life,” says Jurline Redeaux. “I started spotting on a Wednesday, I made an appointment on a Thursday, and I was seeing my doctor on a Friday.”
“Any bleeding, abnormal bleeding, after the age of menopause? Critically important. Do not wait, do not hesitate, the life you save is going to be your own.”
A 2-minute video from Endometrial Cancer Action Network for African Americans (ECANA)
"I worried about not having the time"
“Even though I knew I had an issue with my irregular bleeding periods, being a single mother I worried about not having the time, not having the money,” says Heide.
“I put everything else in front of my health, thinking that I was doing the best thing and I really wasn’t. ” When the bleeding became unbearable and wouldn’t stop, Heide finally sought medical help and was diagnosed with endometrial cancer.
A 2-minute video from Endometrial Cancer Action Network for African Americans (ECANA)
No Screening Test For Endometrial Cancer

“At this time, there are no screening tests or exams to find endometrial cancer early in women who are at average endometrial cancer risk and have no symptoms.”
The American Cancer Society recommends that, at menopause, all women should be told about the risks and symptoms of endometrial cancer and strongly encouraged to report any vaginal bleeding, discharge, or spotting to their doctor.
Source: Can Endometrial Cancer Be Found Early? from the American Cancer Society
"Once You've Reached Menopause, You Should Not Bleed Again"
“Once a woman has gone 12 months without bleeding, any other bleeding is abnormal. And we encourage women to have it evaluated,” says Tashanna Myers, MD, cancer physician at Baystate Health in Massachusetts.
“There’s a misconception that your period can come back, that stress can cause bleeding, but once your periods have gone away and you’ve reached menopause, you should not bleed again.
The reason why the endometrial cancer survival rate is so high is because women have the symptom of bleeding.”
A 2-minute video from Baystate Health.
Genetic Testing and Mutations
Endometrial cancer risk can run in families. Women born with mutations in the genes linked to endometrial cancer have a high lifetime risk and are more likely to develop cancer at a young age. The genes linked to endometrial cancer risk include:

Guidelines for genetic testing in people diagnosed with endometrial cancer
About 5% of women diagnosed with endometrial cancer have an inherited mutation that caused their cancer. There are national guidelines that outline who should consider genetic counseling and testing for an inherited mutation linked to cancer.
Experts recommend that all endometrial cancer tumors have testing to look for an abnormality known as “mismatch repair deficiency” (dMMR) at the time of diagnosis. This abnormality is commonly found in the cancers of people with an inherited gene mutation linked to Lynch syndrome.
People with dMMR cancers are recommended to have genetic counseling and testing for an inherited mutation associated with Lynch syndrome. But not all people with dMMR cancers will test positive for a Lynch syndrome mutation. People with dMMR cancers are recommended to have genetic counseling and testing for an inherited mutation associated with Lynch syndrome. Not all people with dMMR cancers will test positive for a Lynch syndrome mutation.
Genetic counseling and testing for an inherited mutation is also recommended for people diagnosed with endometrial cancer who have any of the following:
- a blood relative with a known inherited mutation in a colorectal cancer gene.
- diagnosed before age 50.
- diagnosed with another Lynch syndrome related cancer including colorectal, ovarian, pancreatic, stomach or other Lynch syndrome-related cancer.
- have a close relative with a Lynch syndrome-related cancer diagnosed under age 50.
- have two or more relatives with a Lynch syndrome-related cancer diagnosed at any age.
- personal history of serous endometrial cancer.
For more information, see “Guidelines for genetic testing in people diagnosed with endometrial cancer” on the FORCE (Facing Hereditary Cancer Empowered) website
Endometrial cancer risk can run in families. Women born with mutations in the genes linked to endometrial cancer have a high lifetime risk and are more likely to develop cancer at a young age. The genes linked to endometrial cancer risk include:
Endometrial Cancer Support Groups
ECANA: Endometrial Cancer Action Network for African-Americans is a group of doctors, patients, survivors, community advocates, and professional leaders “who have come together to create support, community, and empowerment for any African-American affected by endometrial cancer. “
Endometrial Cancer Action Network for African-Americans First National Conference
The Endometrial Cancer Action Network for African-Americans‘ first national conference took place in March 2019 in Honolulu, Hawaii.
The Conference brought together Black women directly affected by endometrial cancer, researchers, clinicians, policy advocates, and reproductive justice leaders for two packed days.
Participants learned about endometrial cancer, shared their stories and the ways they thrived, developed shared frameworks about race and reproductive justice, shared brilliant policy advocacy ideas, laid the groundwork for patient-centered research partnerships, became certified peer educators, and came away with life-long friendships and a growing network!
A 6-minute video about the Conference.
The mission of the Foundation for Women’s Cancer is “to bring together all communities of advocates, patients, caregivers, partners and the healthcare team to eradicate or lessen the impact of gynecologic cancer through research, education and public awareness.”
“Too often, women with endometrial cancer have reported that their symptoms were stigmatized and dismissed. Spot Her is an initiative to help end the silence around endometrial cancer. We aim to embrace the power of every woman’s voice to take a stand on this important women’s health issue. Together we can educate, support, and build strength through community.”
The mission of the Uterine Cancer Awareness Network “is to raise public awareness regarding uterine cancer by informing everyone about the disease! Our vision is to see everyone with a uterus informed about uterine cancer and those diagnosed provided with support services.”
Active Endometrial Cancer Facebook Pages
Endometrial/Uterinal (Womb) Cancer Support and Awareness
Young Women with Endometrial / Uterine Cancer Support Group

Downloads
“If You Have Endometrial Cancer”
A simple guide to endometrial cancer from the American Cancer Society.

“Endometrial Cancer: Your Guide” from the Foundation for Women’s Cancer will take you through the basics about endometrial cancer and introduce the people who may be part of your treatment team. It will also identify the different types of treatments for endometrial cancer.
Two-page fact sheet about uterine cancer from the Centers for Disease Control and Prevention (CDC)
National Comprehensive Cancer Network Guidelines for Patients are developed by the National Comprehensive Cancer Network, an alliance of leading cancer centers across the United States devoted to patient care, research, and education. The Guidelines present information in an easy-to-learn format for people with cancer and those who support them and explain the cancer care options likely to have the best results.
Reports
American Cancer Society. American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.

American Association for Cancer Research: Cancer Disparities Research Report 2020
American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020. Atlanta: American Cancer Society, 2018