Cervical Cancer Disparity Facts
- more likely to be diagnosed with cervical cancer
- more likely to be diagnosed at a later stage of cervical cancer
- less likely to receive optimal treatment
- nearly twice as likely to die of cervical cancer
- more likely to be diagnosed with cervical cancer
- more likely to die of cervical cancer

NA=Native American 10.1, H=Hispanic 10.0,
B=Black 9.0, W=White 7.1, A=Asian/Pacific Islander 6.3
Source: National Cancer Institute Cancer
Stat Facts: Cervical Cancer
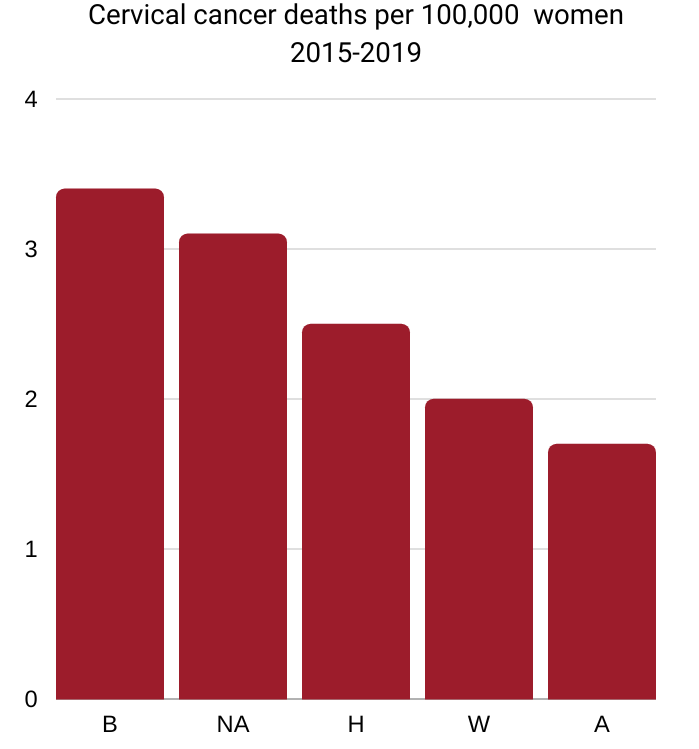
B=Black 3.4, NA=Native American 3.1,
H=Hispanic 2.5, W=White 2.0, A=Asian/Pacific Islander 1.7
Source: National Cancer Institute Cancer
Stat Facts: Cervical Cancer
Incidence
Black women. The incidence rate of cervical cancer is 22% higher in Black women than in White women. However, the disparity is much wider when rates exclude women who cannot develop cervical cancer because of a hysterectomy (removal of uterus and cervix), a procedure more common in Black women. One study found that after correcting for hysterectomy, incidence for cervical cancer was approximately 40% higher in Black than White women. From 2009-2018, cervical cancer incidence rates among Black and White women were stable.
Source: American Cancer Society Cancer Facts & Figures for African American/Black People 2022-2024.
Hispanic women. The cervical cancer incidence rate among US Hispanic women is nearly 40% higher than among white women.
Source: American Cancer Society Cancer Facts & Figures for Hispanics/Latinos 2018-2020. Atlanta: American Cancer Society, 2018
Hispanics have a higher rate of cervical cancer compared with Whites. Hispanic women have an approximately 43 percent higher risk of cervical cancer incidence compared to White women.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022.
Hispanic women have a significantly higher incidence rate of cervical cancer and slightly higher mortality rate, with especially high rates occurring along the Texas-Mexico border.
Source: U.S. Preventive Services Task Force. Cervical Cancer: Screening (2018)
American Indian/Alaska Native. Compared to White people, AI/AN people had a higher incidence rate during 2014-2018 for cervical cancer.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022.
Screening
Black women. Several studies have found that African American women are screened for cervical cancer at rates similar to those for white women and that inadequate follow-up after screening and differences in treatment may be important contributing factors for their greater rate of mortality.
Source: American Cancer Society. Cancer Facts & Figures for African Americans 2019-2021. Atlanta: American Cancer Society, 2019
Asian American women. Asian women also have lower screening rates, especially those who have recently immigrated to the United States and may have language or cultural barriers to screening.
Source: U.S. Preventive Services Task Force. Cervical Cancer: Screening (2018)
Strains of HPV
Hispanic women. Cervical cancer is caused by persistent infection with certain strains of HPV. These carcinogenic strains of HPV have a higher prevalence among Hispanic women.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022.
Tumor type
Black women.The higher mortality rate in African American women may be attributable, in part, to the higher than average rate of adenocarcinoma, which carries a worse prognosis than the most common type of cervical cancer (squamous cell carcinoma).
Source: U.S. Preventive Services Task Force. Cervical Cancer: Screening (2018)
Stage at diagnosis
Black women. Racial differences in stage at diagnosis may be due to differences in the quality of screening and/or follow-up after abnormal results. Black women have lower survival than White women for every stage of diagnosis, likely reflecting disparities in access to care and receipt of high-quality treatment.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Black women are more likely than white women to be diagnosed with regional- or distant-stage disease. This may be due to differences in the quality of screening and follow-up after abnormal results. Lower socioeconomic status and lack of health insurance are also associated with lower screening rates and increased risk of late-stage diagnosis.
Source: American Cancer Society. Cancer Facts & Figures for African Americans 2019-2021. Atlanta: American Cancer Society, 2019
Hispanic women. The proportion of Hispanic women with cervical cancer who are diagnosed with localized disease is slightly lower than that in non-Hispanic whites (42% versus 44%, respectively).
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020. Atlanta: American Cancer Society, 2018
Treatment
Black women. Black women have lower survival than White women for every stage of diagnosis, likely reflecting disparities in access to care and receipt of high-quality treatment. For example, one study found that among people diagnosed with early-stage disease, 17% of Black women did not receive surgery compared to just 9% of White women. Further, Black women are less likely to receive recommended radiation therapy for every stage of disease.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Treatment differences accounted for 47% of black-white differences in cervical cancer mortality. Lack of health insurance may explain 19% of the excess risk for blacks. Among early-stage cervical cancer patients, a greater proportion of black women (17%) failed to receive surgery, which is the standard of care, compared to white (9%) and Hispanic (12%) women.
Source: American Cancer Society. Cancer Facts & Figures for African Americans 2019-2021. Atlanta: American Cancer Society, 2019
5-year survival
Black women. The overall 5-year relative survival rate for cervical cancer among Black women is 56%, compared to 67% among White women, partly because Black women are more likely to be diagnosed with regional- or distant-stage disease.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Hispanic women. Five-year survival for cervical cancer is 72% among Hispanic women and 70% among non-Hispanic whites.
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020. Atlanta: American Cancer Society, 2018
Mortality
Black women. Cervical cancer death rates have declined steadily since the 1970s , mostly as a result of screening. Rates in Black women continued to decline by 2% per year from 2010 through 2019, but have stabilized in White women in recent years. Despite this progress, Black women remain 65% more likely to die from cervical cancer than White women, with an even larger disparity after rates are corrected for hysterectomy prevalence.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
The overall mortality rate from cervical cancer among African American women is more than twice the rate among white women (when adjusted for hysterectomy rate since this procedure removes the cervix). Mortality is higher among older African American women.
Source: U.S. Preventive Services Task Force. Cervical Cancer: Screening (2018)
Hispanic women. Despite steady declines, death rates in Hispanic women during 2012-2016 remained 26% higher than those in whites.
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020. Atlanta: American Cancer Society, 2018.
Hispanic women have about a 20 percent higher risk of death from cervical cancer compared to White women.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022.
White women. Although white women overall have the lowest mortality rate from cervical cancer, white women living in geographically isolated and medically underserved areas (particularly Appalachia) have much higher mortality rates than the US average.
Source: U.S. Preventive Services Task Force. Cervical Cancer: Screening (2018)
American Indian/Alaska Native women. American Indian/Alaska Native women have higher rates of cervical cancer mortality than the US average. Factors driving this higher rate may include (1) lower screening rates, with 16.5% of American Indian/Alaska Native women in 2012 reporting not receiving a Pap test in the past 5 years and (2) inadequate follow-up.
Source: U.S. Preventive Services Task Force. Cervical Cancer: Screening (2018)
An average of 11 women die of cervical cancer each day in the United States. Half of them are in their 50s or younger.
Source: Cancer statistics, 2022. American Cancer Society.
Why are Black women more likely to die from cervical cancer?
“There really isn’t a genetic difference that is causing Black women to die at higher rates of cervical cancer,” says Olivia Cardenas-Trowers, MD, a Mayo Clinic urogynecologic surgeon.
“It has to do more with systemic racism. These disparities started way back when and have infiltrated the healthcare system and affected women’s access to resources and the health care that they need. This trickles down into poor outcomes.”
“Transportation, health literacy, even trust in their provider because of injustices that have happened in the past, these things affect their health care.”
“Black women may not undergo the typical screening that could catch a abnormality earlier and therefore these cancers may be diagnosed at later stages when the likelihood of mortality is higher. Also, they may have problems getting access to treatment. They may not have the finances to be able to undergo surgery, or chemo or radiation. So all of these can factor into the increased mortality in Black women.”
A 7-minute video from the Mayo Clinic
“There are not enough Black women sharing their stories and I get why because there’s so much stigma involved”
“When I was a little girl growing up, I didn’t think one day I’m going to be talking about HPV and cervical cancer,” Tamika Felder says about being a 22-year cervical cancer survivor.

“There are not enough Black women sharing their stories, and I get why because there’s so much stigma involved in it,” she says. “When we talk about vaginal health, in a lot of cultures and communities it’s taboo to talk about those things. But the problem when we don’t talk about them is that more people are dying.”
Two things can be done to lower the risk of cervical cancer for Black women, says Karen Patricia Williams, PhD., of Ohio State University.
The first is that the healthcare system has to follow up with women who have abnormal Pap tests.
The second is that women should not to jump to conclusions about what an abnormal test result means. “It doesn’t mean that you are a whore,” she says. “At the end of the day, who cares what these people think, because you’re talking about your health.”
Source: “What Black Women Need to Know About Cervical Cancer” on the Word in Black website (September 12, 2022)
How the rate of cervical cancer varies by states

The darker the blue color, the higher the rate of cervical cancer per 100,000 women. The states with the highest rates are Oklahoma, Wyoming and Alabama.
Source: Cancer Statistics At a Glance (CDC)
A Preventable Cancer Is on the Rise in Alabama

The state’s refusal to expand Medicaid is causing poor women to miss out on lifesaving screenings.
Women who develop cervical cancer in Alabama are more likely to die than their counterparts in any other state—and in recent years Alabama’s mortality rate has been rising.
In 2014, when Medicaid expansion took hold under the Affordable Care Act, Alabama and twenty-four other states, almost all of which had Republican-led legislatures, opted out.
A Human Rights Watch report found that Alabama women without medical insurance routinely delayed getting care, “which, for some, meant that gynecological cancers weren’t found until symptoms developed to more advanced stages.”
Source: “A Preventable Cancer Is on the Rise in Alabama” by Eyal Press on the New Yorker website (March 30, 2020)
Georgia Black women traumatized by neglect and abuse by physicians
“I conducted over 20 interviews with Black women from South Georgia about their experiences accessing reproductive healthcare, as well as their knowledge about the cervical cancer disease and prevention,” says Olivia Coley Pearson.
 “As I anticipated, lack of medical insurance, as well as lack of reproductive and obstetrical and gynecological services located in rural counties were among the substantial barriers faced by most rural women with limited or no reliable transportation, as well as inadequate broadband (if at all) and other sources of public information.
“As I anticipated, lack of medical insurance, as well as lack of reproductive and obstetrical and gynecological services located in rural counties were among the substantial barriers faced by most rural women with limited or no reliable transportation, as well as inadequate broadband (if at all) and other sources of public information.
However, I was continuously astonished by stories that revealed the extent to which women were traumatized by the worst kind of neglect and abuse at the hands of physicians who were less compassionate or lacked the resources and training needed to equitably treat all patients.
Internalized trauma has led to decades of generational mistrust and fear. Some women shared that they didn’t talk to doctors about their reproductive health because of mistrust of doctors and the system.”
Pearson, a community-based researcher for Southern Rural Black Women’s Initiative and Human Right Watch, is the first Black woman elected city commissioner of Douglas, Georgia.
Source: “Black women die disproportionately from preventable cervical cancer” by Olivia Coley Pearson in the Meridian Star website (Feb 18, 2022)
Highest rate of cervical cancer in Oklahoma is American Indians

The overall rate of cervical cancer is on the decline in the US, but in Oklahoma, particularly in rural communities, the cases are increasing.
Debra Richardson, M.D., gynecologic oncologist from OU Health Stephenson Cancer Center, explains that lack of access to healthcare could mean that rural Oklahomans are experiencing a higher cervical cancer mortality rate. Those in communities with limited access to healthcare and screening are being diagnosed with metastatic cervical cancer.
Despite the HPV vaccine and regular screening reducing cervical cancer rates across the nation, the rate of Oklahomans taking the vaccine are low. “Our HPV vaccine rate is 48th out of 50 in the nation and for screening we are number 45 out of 50,” Dr. Richardson said.
Sadly, the highest rate of cervical cancer in Oklahoma is American Indians at five for every 100,000 women. Dr. Richardson points to the lack of access to care being the primary issue for these alarming rates.
Source: “Beating Cervical Cancer in Oklahoma” on the website of Oklahoma University Health (September 22, 2022)

In the state of Georgia, Black women are almost one and a half times as likely to die of cervical cancer as white women and these disparities increase at alarming rates as they age. Black Georgian women are more likely to have never been screened for cervical cancer, are diagnosed at a later stage, and have lower five-year survival rates.
Georgia state and local agencies, and the US federal government are not doing enough to facilitate access to reproductive healthcare services and information to prevent cervical cancer deaths and address racial disparities in health outcomes.
Georgia does not ensure access to comprehensive and affordable reproductive health care, and instead relies on a patchwork of multiple, publicly funded programs to extend healthcare coverage to low-income women in the state, including for gynecological care. Georgia has not expanded Medicaid through the US Affordable Care Act (ACA) to extend healthcare coverage to more low-income individuals, for which the state is losing out on $3 billion in federal funding each year. Over 255,000 Georgians have no options for affordable healthcare coverage.
Without a comprehensive plan to guarantee access to consistent and affordable health care, the state has left low-income and uninsured Georgian women—who are more likely to be Black—struggling to navigate gaps in health insurance coverage and enormous financial barriers to cervical cancer care.
For many women, especially those who are uninsured, their inability to afford reproductive healthcare services means that they often avoid medical appointments and skip cancer screenings and follow-up care altogether, forgoing lifesaving opportunities to prevent and treat the disease.
Source: “We Need Access: Ending Preventable Deaths from Cervical Cancer in Rural Georgia” by the Human Rights Watch on the Human Rights Watch website (2022)
Update: Racial Disparities Persist in Efforts to Eradicate Cervical Cancer

By Annerieke Smaak Daniel
Since 2018, Human Rights Watch has documented barriers that are fueling racial disparities in cervical cancer death rates in rural communities in the South, first in Alabama and then more recently in Georgia in partnership with the Southern Rural Black Women’s Initiative for Economic and Social Justice.
Our research points to clear patterns of neglect, exclusion, and discrimination that prevent Black women in rural and underserved communities from accessing affordable, comprehensive, and equitable reproductive health-care services and information. Our research also shows that the US government and state governments can help eliminate these inequalities.
We spoke with women in Alabama and Georgia, the majority of whom were uninsured and living in poverty, who described how they couldn’t afford to pay for cervical cancer care. They said they often had to make difficult choices, sometimes choosing between buying groceries or paying their utility bills or getting the health care they needed.
The racial disparities we see in cervical cancer outcomes are an example of the ways that racial discrimination perpetuates health inequalities in our country. US federal and state governments need to take steps to dismantle racism and address the ways that discrimination and inequality impede the rights to health, information, and equality for everyone.
See “Racial Disparities Persist in Efforts to Eradicate Cervical Cancer” by Annerieke Smaak Daniel on the Human Rights Watch website (February 8, 2023)
Hispanics and Cervical Cancer
Why Hispanic Women Are Still Dying From A Curable Cervical Cancer
by Sarah Felbin
A lack of health insurance prevents some from regular physician visits. Language is often another obstacle. For women who aren’t proficient in English, medical jargon and pamphlets can be frustrating to receive.
Girls grow up without receiving proper sex education, resulting in a lack of self-care, a lack of information towards their body, and their overall health.
There’s also the cultural expectation that a woman’s role is to be in charge of the household. Especially in the Latino community, you do everything, you put yourself last, you have to take care of everyone else’s needs.
See: “Why Hispanic Women Are Still Dying From A Curable Cancer” by Sarah Felbin on the Women’s Health magazine website (October 15, 2021)
