Lung cancer disparity facts
Compared with White men, Black men are:
- more likely to be diagnosed with lung cancer
- less likely for lung cancer to be diagnosed at an early stage
- less likely to receive optimal surgical treatment
- more likely to receive no treatment
- more likely to die from lung cancer
Compared with White women, Black women are:
- less likely to be diagnosed with lung cancer
- less likely for lung cancer to be diagnosed at an early stage
- less likely to receive optimal surgical treatment
- more likely to receive no treatment
- less likely to die from lung cancer
Compared with White men women, Hispanic men and women are:
- less likely to be diagnosed with lung cancer
- less likely for lung cancer to be diagnosed at an early stage
- more likely to receive no treatment
- less likely to die from lung cancer
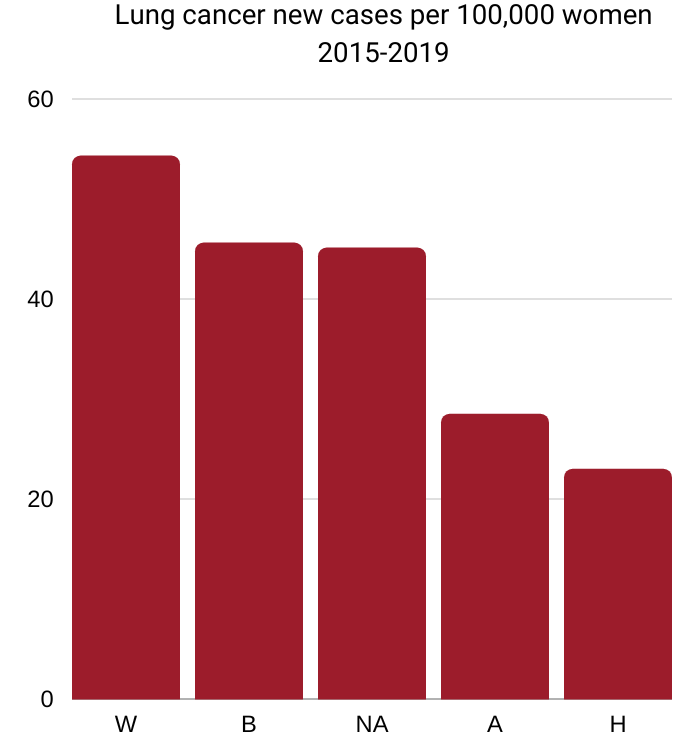
W=White 54.3, B=Black 45.6,
NA=Native American 45.1, A=Asian/Pacific Islander 28.5, H=Hispanic 23.0
Source: National Cancer Institute Cancer
Stat Facts: Lung and Bronchus Cancer
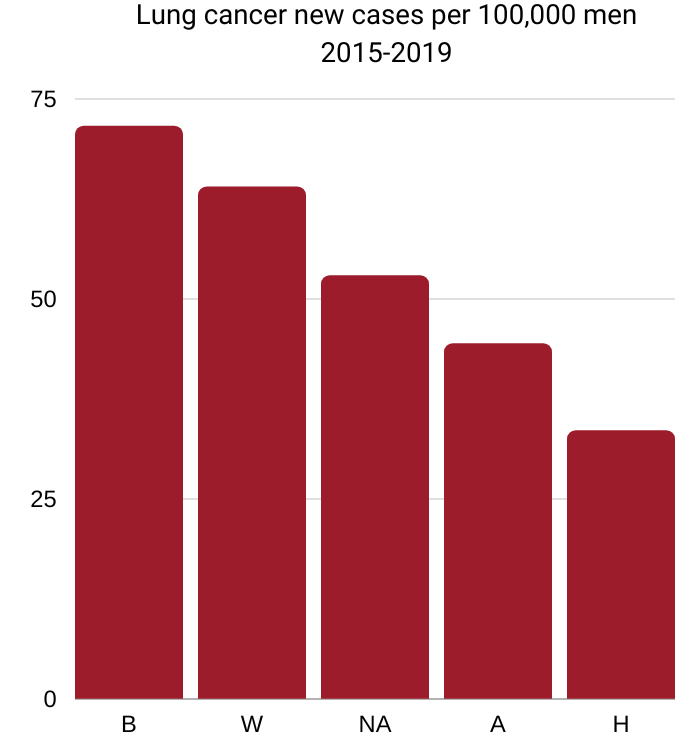
B=Black 71.6, W=White 64.0,
NA=Native American 52.9, A=Asian/Pacific Islander 44.4, H=Hispanic 33.5
Source: National Cancer Institute Cancer
Stat Facts: Lung and Bronchus Cancer
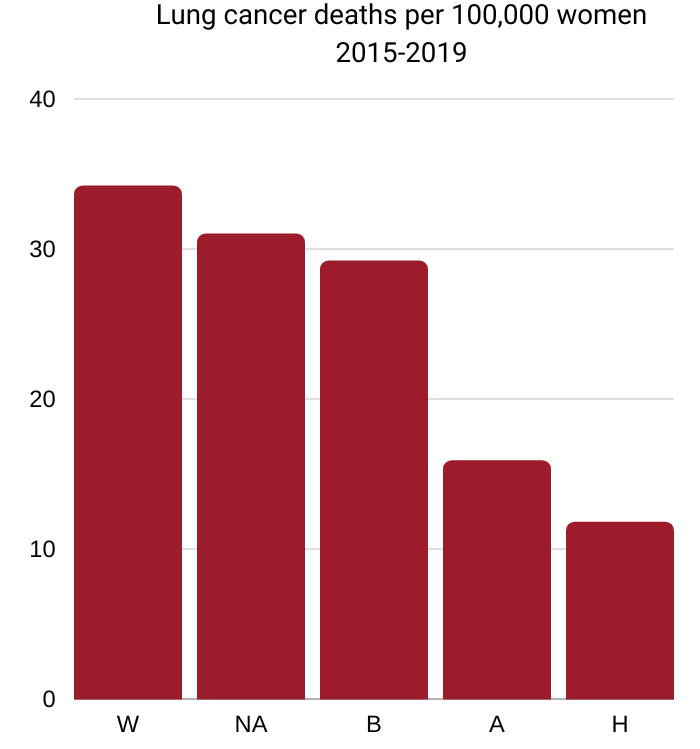
W=White 34.2, NA=Native American 31.0,
B=Black 29.2, A=Asian/Pacific Islander 15.9, H=Hispanic 11.8
Source: National Cancer Institute Cancer
Stat Facts: Lung and Bronchus Cancer
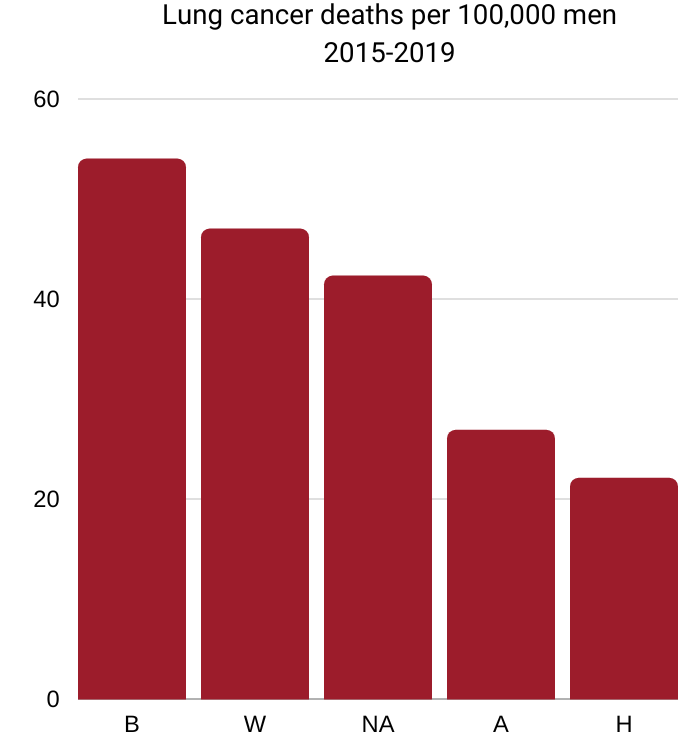
B=Black 54.0, W=White 47.0,
NA=Native American 42.3, A=Asian/Pacific Islander 26.9, H=Hispanic 22.1
Source: National Cancer Institute Cancer
Stat Facts: Lung and Bronchus Cancer
Incidence
Black men and women. During 2014-2018, incidence rates were 12% higher in Black men than in White men but 16% lower in Black women than in White women. Similar to White men, incidence rates in Black men increased rapidly until the mid-1980s because of widespread smoking uptake during the first half of the 20th century, but have since declined steadily due to reductions in smoking. In contrast, rates in Black women increased until the late 2000s before declining because of later and slower smoking uptake and cessation compared to men.
Steeper smoking declines in Black people than in White people have resulted in a convergence in lung cancer incidence among young Black and White men and a crossover among women. From 2009 to 2018, the annual decline in incidence was about 3% in Black and White men, 2% in Black women, and 1% in White women.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Effective smoking cessation campaigns over the past five decades have resulted in a steady decline in the overall lung cancer incidence with a steeper decline among Black adults, greatly reducing the disparity in lung cancer incidence between Black and White populations. Despite the narrowing disparities, lung cancer incidence rates in Black men were 12 percent higher than those in White men during 2014-2018.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022.
Hispanic men and women. Lung cancer incidence rates among Hispanics are about half those of whites because of traditionally lower cigarette smoking prevalence and because Hispanic smokers are less likely to smoke daily and more likely to smoke fewer cigarettes overall. From 2006 to 2015, lung cancer incidence rates in men declined by 2.0% annually among Hispanics, similar to declines among whites. A recent study reported a decline of about 1% annually for Hispanic women over the past five years, similar to the trend in white women.
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020.
Hispanics have a lower rate of lung cancer compared with Whites. Because of the heterogeneity of the Hispanic population, the risk for different cancer types varies widely depending upon country or region of ancestral origin. Lung cancer incidence rates during 2014-2018 among Hispanics in Puerto Rico were 44 percent lower than among Hispanics in the mainland U.S.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022.
American Indian/Alaska Native (AI/AN). Compared to White people, AI/AN people had a higher incidence rate during 2014-2018 for lung cancer. Furthermore, AI/AN populations living in different Purchased/Referred Care Delivery Area (PRCDA) regions (tribal areas or surrounding counties) have substantially different cancer risk and disparities compared to each other and to the White population. AI/AN individuals living in the Northern Plains PRCDA region have five times higher incidence of lung cancer—the most diagnosed cancer in the AI/AN population—than those living in the Southwest PRCDA region. When compared to White individuals, the lung cancer incidence is 80 percent higher among AI/AN individuals living in the Northern Plains, but 64 percent lower in those living in the Southwest.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022
Native Hawaiians. Although Hawaii had among the lowest rates of lung cancer in the US in 2012-2016, lung cancer incidence was highest among Native Hawaiian men and women, and lung cancer mortality was highest in Native Hawaiian women compared to the other population groups in the state.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022
Smoking
Hispanic men and women. While smoking prevalence in Hispanics overall is substantially lower than in whites, among Puerto Ricans living in the States it is currently similar to whites.
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020.
Diagnosis
Black men and women. Both Black men and women are more likely to be diagnosed with lung cancer at a younger age than Whites, with a median age at diagnosis of 67 versus 71, respectively. Localized-stage lung cancer is only diagnosed in 21% of Black people and 25% of White people because symptoms generally do not appear until the disease is advanced.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
For those with lung cancer, compared with white Americans, Black Americans were 16% less likely to be diagnosed early, Latinos 13% less likely, Asian Americans or Pacific Islanders 15% less likely, and American Indians/Alaska Natives 14% less likely to be diagnosed early with lung cancer.
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020.
Black Americans with lung cancer were 15% less likely to be diagnosed early compared to White Americans.
Source: State of Lung Cancer 2022 (American Lung Association)
While 25% of Whites are diagnosed with lung cancer in its early stages, only 21% of Blacks, 22% of Hispanics, 21% of Asian Americans and Pacific Islanders, and 22% of Anerican Indians and Alaska Natives are.
Source: “State of Lung Cancer 2021 Report” (American Lung Association)
Hispanic men and women. Most Hispanic patients with lung cancer are diagnosed at an advanced stage. Only 17% of Hispanics are diagnosed with localized disease, for which the 5-year cause-specific survival is 63%, dropping to 34% and 6% for regional and distant stage disease, respectively.
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020.
Latino Americans with lung cancer were 15% less likely to be diagnosed early compared to White Americans.
Source: State of Lung Cancer 2022 (American Lung Association)
Asian Americans or Pacific Islanders with lung cancer were 16% less likely to be diagnosed early compared to White Americans.
Source: State of Lung Cancer 2022 (American Lung Association)
American Indians and Alaska Natives with lung cancer were 13% less likely to be diagnosed early compared to White Americans.
Source: State of Lung Cancer 2022 (American Lung Association)
Clinical trials
Black and Hispanics are under-represented in clinical trials that look at biomarkers which can help identify appropriate personalized treatments. Whites and Asians are over-represented in these trials.
Source: “Racial and Ethnic Disparities Among Participants in Precision Oncology Clinical Studies” by Christopher M. Aldrighetti et al. (November 8, 2021).s
Treatment
Black men and women. Numerous studies have shown that even when lung cancer is diagnosed early, Black people are less likely than White people to receive surgery, which is the most effective treatment for survival. When treatment is equivalent, outcomes are similar between Black and White individuals.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
One recent study of early-stage lung cancer patients found that surgery was less often recommended for black lung cancer patients compared to other racial/ethnic groups, and as a result, 47% of Black patients did not receive surgical treatment compared to 38% of Hispanics and Whites and 34% of Asians. In contrast, another study found that racial differences in receipt of surgery were eliminated in 2010 for early-stage lung cancer patients treated at Veterans Affairs facilities, and in fact there were no differences in survival outcomes between Blacks and whites in the equal access health care system.
Source: American Cancer Society. Cancer Facts & Figures for African Americans 2019-2021. Atlanta: American Cancer Society, 2019.
While 21% of Whites and Hispanics receive surgical treatment for lung cancer, only 17% of Blacks and 17% of Anerican Indians and Alaska Natives do. In contrast, 24% of Asian Americans and Pacific Islanders receive surgical treatment.
Source: “State of Lung Cancer 2021 Report” (American Lung Association).
Black Americans with lung cancer were 19% less likely to receive surgical treatment compared to White Americans.
Source: State of Lung Cancer 2022 (American Lung Association)
Latino Americans with lung cancer were equally likely to receive surgical treatment compared to White Americans.
Source: State of Lung Cancer 2022 (American Lung Association)
Asian Americans or Pacific Islanders with lung cancer were 16% more likely to receive surgical treatment compared to White Americans.
Source: State of Lung Cancer 2022 (American Lung Association)
American Indians and Alaska Natives with lung cancer were 21% less likely to receive surgical treatment compared to White Americans.
Source: State of Lung Cancer 2022 (American Lung Association)
Black Americans were 10% more likely, Latino Americans 28% more likely, Asian Americans or Pacific Islanders 3% more likely, and American Indians and Alaska Natives 11% more likely to not receive any treatment for their lung cancer compared to White Americans.
Source: State of Lung Cancer 2022 (American Lung Association)
5-year survival
Black men and women. The 5-year relative survival rate for lung cancer is slightly lower in Black people than in White people overall, 20% versus 22%, with the largest difference for localized-stage disease (55% versus 60%). Localized-stage lung cancer is only diagnosed in 21% of Black people and 25% of White people because symptoms generally do not appear until the disease is advanced.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Blacks were 21% less likely than Whites to survive 5 years after diagnosis, Hispanics 16% less likely, and American Indians/Alaska Natives 13% less likely. ON the other hand, Asian Americans and Pacific Islanders were 9% more likely to survive 5 years.
Source: “State of Lung Cancer 2021 Report” (American Lung Association).
From 2000 to 2017, the median survival time for Black patients increased only about 25%, well below the 39% increase in White patients and the 98% increase in Asian and other non-White/non-Black patients. Among lung cancer patients diagnosed in 2017, Asian and other non-White/non-Black patients survived a median of about 20 months, White patients about 14 months, and Black patients 12 months.
Source: Prognosis and Survival Analysis of 922,317 Lung Cancer Patients from the US Based on the Most Recent Data from the SEER Database (April 15, 2021)
Black Americans with lung cancer were 12% less likely to survive five years compared to White Americans.
Source: State of Lung Cancer 2022 (American Lung Association)
Hispanic men and women. The 5-year cause-specific survival after diagnosis with localized disease is 63% for Hispanics, dropping to 34% and 6% for regional and distant stage disease, respectively. Similar to whites, Hispanic women have higher 5-year lung cancer survival than Hispanic men (25% versus 16%), partly because women are more frequently diagnosed at an early stage. However, women have higher survival rates than men for every stage of diagnosis.
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020.
Latino Americans with lung cancer were 25% less likely to survive five years compared to White Americans.
Source: State of Lung Cancer 2022 (American Lung Association)
Asian Americans or Pacific Islanders with lung cancer were equally likely to survive five years compared to White Americans.
Source: State of Lung Cancer 2022 (American Lung Association)
American Indians and Alaska Natives with lung cancer were 23% less likely to survive five years compared to White Americans.
Source: State of Lung Cancer 2022 (American Lung Association)
Mortality
Black men and women. Lung cancer is the leading cause of cancer death in Black men and the second-leading cause in Black women. After increasing for decades, lung cancer death rates have declined since 1990 at a generally faster pace in Black men than in White men, reducing the racial disparity from an excess of 40% in Black men in 1990-1992 to 15% in 2015-2019. In women, the downturn began about a decade later than that in men and is also steeper in Black than White women. Consequently, although Black and White women had similar lung cancer mortality until the early 1990s, in 2015-2019 rates were 15% lower in Black women.
The more favorable trends among Black people reflect the steep decline in smoking initiation unique to Black youth from at least the mid-1970s until the early 1990s. During 2015-2019, the lung cancer death rate declined by about 6% per year in Black men, 5% per year in White men, and 4% per year in Black and White women. These accelerated trends reflect recent advances in lung cancer treatment, as well as reductions in smoking.
Source: American Cancer Society. Cancer Facts & Figures for African American/Black People 2022-2024.
Lung cancer is also the leading cause of cancer-related mortality in Black men and the second-leading cause of cancer deaths in Black women. Encouragingly, the lung cancer-related mortality has declined at a faster pace in Black individuals than in White individuals over the past two decades. During 2015-2019, the most recent period for which such data are available, the lung cancer death rate declined by about six percent every year in Black men compared to five percent in White men, and four percent in Black and White women. These trends reflect a steep decline in smoking rates over the past five decades, thanks to effective public health policies.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022.
Hispanic men and women. Lung cancer is the leading cause of cancer death among Hispanic men and the second-leading cause among Hispanic women. From 2007 to 2016, death rates for lung cancer declined by 3.5% per year among Hispanic men, very similar to declines among white men, and by 1.4% per year among Hispanic women, compared to 2.3% per year among white women. The steeper decline among men reflects earlier and larger reductions in smoking compared to women, who took up smoking in large numbers about 20 years after men.
Lung cancer death rates within Hispanic subpopulations vary substantially by country of origin, particularly among men, reflecting differences in historical smoking patterns. In one study in Florida, lung cancer death rates in Cuban men, who have the heaviest smoking history among Hispanic subgroups, were nearly 50% higher than those in Puerto Rican men during 2008-2012.
Source: American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2018-2020.
Asian Men and Women. Of the cancer types common in the overall U.S. population, lung cancer is the leading cause of cancer-related deaths in the Asian population. Furthermore, Asian individuals, particularly women without a history of smoking, have a uniquely high burden of lung cancer among never-smokers. Notably, more than 30 percent of lung cancer patients in Asia, including more than half of female patients with lung cancer, are never‐smokers. This observation has been attributed to a markedly increased rate of epidermal growth factor receptor (EGFR)–mutant lung cancer in Asian female nonsmokers.
Source: American Association for Cancer Research Cancer Disparities Progress Report 2022.
"Number one, disparities are preventable..."
“Number two, disparities are incredibly costly. The third thing is that as we begin to focus on preventing, narrowing, and eliminating disparities, we have to understand that the solutions come from multiple levels,” says Raymond U. Osarogiagbon, MD, of the Baptist Cancer Center in Memphis, Tennessee.
 The least effective is the level of blaming the victims of disparities. Patients don’t go in with the idea that they will do something to hurt themselves. A patient with lung cancer who is poor, does not stand up in the morning and decide, “I am so going to make sure I get the wrong treatment today. I don’t care if I die.”
The least effective is the level of blaming the victims of disparities. Patients don’t go in with the idea that they will do something to hurt themselves. A patient with lung cancer who is poor, does not stand up in the morning and decide, “I am so going to make sure I get the wrong treatment today. I don’t care if I die.”
Where is our intervention most successfully deployed? I think it is important to recognize that the level at which we can have the most impact is at the policy level. The second biggest level of impact is at the organizational level.
When we talk about disparities, I think it is very important for us to get away from the traditional narrow lens that asks, “Who are these people or why do they have such terrible outcomes?” We should recognize that we have seen the enemy, and it is us [the medical establishment].”
Source: “Addressing Disparities in Lung Cancer from a Geographic Perspective” by Tony Berberabe.
See also “Unequal Resource Distribution Underlies Lung Cancer Disparities” by M. Alexander Otto.
Patients go to the Doctor only when they're unwell, which is too late
“Many people don’t think it’s cancer until they notice a problem,” says Illinois cancer physician Shaina Rozell.
“So, it’s not until I’m coughing up blood or developing pain that I’m actually seeking care. Whereas lung cancer screenings are more for when you are feeling well and healthy. Most patients are not going to the doctor when they’re feeling healthy. They go to the doctor when they’re feeling unwell.”
“Unfortunately, because of that, we’re diagnosing these lung cancer cases at later stages.”
A 1-minute video from MD Newsline.
A cure no longer exists for some of these patients at stage 3 and 4
“The options for surgery during later stages of lung cancer are pretty limited,” says Illinois cancer surgeon Shaina Rozell. “You do surgery at stage one or stage two, but most of these patients, they’re presenting at stage three or stage four. So the potential for cure no longer exists for these patients.”
“Because of that you see a major disparity between African Americans and non-African Americans in being diagnosed and having surgeries. Unfortunately, because of that, we’re diagnosing these lung cancer cases at later stages.”
A 1-minute video from MD Newsline.
