Clinical Trials About
What are clinical trials?
Cancer clinical trials allow researchers to study innovative and potentially life-saving new treatments. The goal is to find treatments that are better than what’s currently available.
Placebos are rarely used in cancer treatment clinical trials. If participants don’t receive the study medication, they are always given the best available treatment for their particular cancer. This helps the researchers determine whether the study medication is better than the standard treatment.
A 2-minute video from Stand Up to Cancer

Cancer clinical trials allow researchers to study innovative and potentially life-saving new treatments. The goal is to find treatments that are better than what’s currently available.
Placebos are rarely used in cancer treatment clinical trials. If participants don’t receive the study medication, they are always given the best available treatment for their particular cancer. This helps the researchers determine whether the study medication is better than the standard treatment.
A 2-minute video from Stand Up to Cancer
Source: Stand Up to Cancer
Hi, my name is Dr Jonathan Jackson. I’m the founder and executive director of the Community Access Recruitment and Engagement or Care Research Center at Massachusetts General Hospital and Harvard Medical School.
I’ve designed and run clinical trials but more importantly, I’ve also participated as a study volunteer in dozens and dozens of research studies. So I’ve been on both sides of the clinical research process.
Clinical research awareness is important because I believe that the only way new cures and treatments work for everyone is if everyone gets involved in the process.
So throughout this video, my goal is to tell you more about clinical trials and help answer questions you may have about participation.
All clinical trials begin with a question that scientists, including doctors and disease experts, want to answer. Scientists prepare a development plan based on early studies done in the lab.
Next researchers submit a request to regulatory and government agencies like the U. S. Food and Drug administration to begin testing a new therapy in people. Once this request is approved, researchers seek volunteers to participate in clinical trials.
The success of these trials depends on including a diverse group of people representative of those who may be treated by the new therapy if it is approved for use.
There are four phases of clinical trials: to check the safety of the treatment, see how it works in participants with specific medical conditions, check how well it works in a larger group of people, and see how the therapy works in the real world and its long term effects.
This whole process could take over eight years. This development process is important because it’s the best way to ensure that the safest, most effective therapies reach the public.
A 9-minute video from CISCRP
Cancer clinical trials allow researchers to study innovative and potentially life-saving new treatments. The goal is to find treatments that are better than what’s currently available.
Placebos are rarely used in cancer treatment clinical trials. If participants don’t receive the study medication, they are always given the best available treatment for their particular cancer. This helps the researchers determine whether the study medication is better than the standard treatment.
A 2-minute video from Stand Up to Cancer
Reason one. You have a chance to receive treatment based on the latest research that is not yet available to others. Clinical trials are based on the best knowledge available for your kind of cancer.
Reason two. You’ll get high-quality care and be carefully monitored throughout the study.
Reason three. You add to the world’s knowledge about cancer and help to improve cancer care for future generations.
A 2-minute video from the National Cancer Institute
An overview of clinical trials

Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
“We do clinical trials in order to understand processes that are involved in lung cancer, whether that’s the treatments that are effective or whether they’re safe,” says Manish Patel, D.O., and oncologist and researcher at the University of Minnesota.
“It really is the clinical trial that determines how we take care of patients. All of these clinical trials are involved in developing the best therapy for patients with lung cancer.
Without clinical trials, we really don’t know what the best treatments are or how to choose the treatment for a patient with with lung cancer.
So they’re incredibly important.”
A 1-minute video from You and Lung Cancer
Lung cancer clinical trials are research studies in which people volunteer to help test new treatments, procedures or ways to diagnose or screen for lung cancer. Clinical trials help researchers develop better tests and treatments and are especially important in lung cancer.
What is a clinical trial? Why are clinical trials need in lung cancer?
What are pre-clinical studies? Who is in charge of clinical trials?
Who approves treatments after clinical trials?
What are Phases 1, 2, 3, 4 of a clinical trial?
Who can be in a lung cancer clinical trial? How can I join a lung cancer clinical trial?
What is informed consent? Can I leave a clinical trial after I join?
What are the benefits and risks of taking part in a clinical trial?
A 6-minute video from You and Lung Cancer
Clinical Trials Diversity Importance
McCaskill-Stevens: Diversity ‘critical’ in clinical trials
A 3-minute video from the Washington Post
Ask Ruby: Why is Diversity Important in clinical trials?
A 2-minute video from the Cancer Support Community

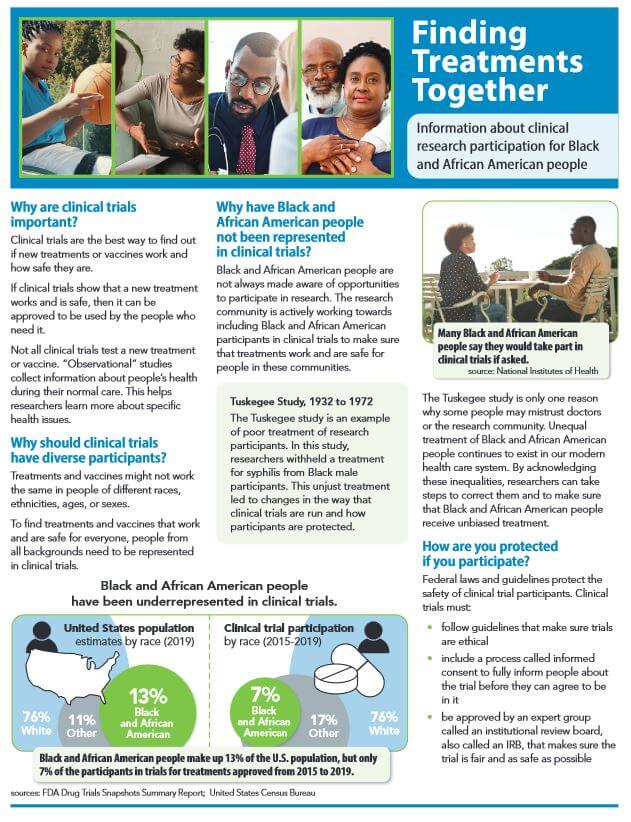
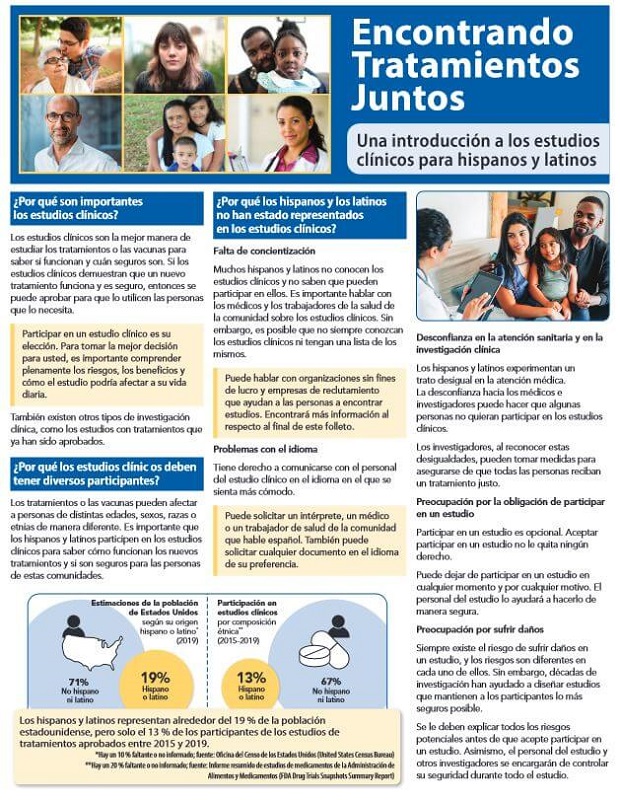
A free 8-page brochure about clinical trials and the benefits, concerns, facts, barriers, importance of diversity, participation, tips and resources.
Source: Cancer Support Community
Lack of diversity one reason why Black women have worse breast cancer outcomes?
Not being included in clinical trials may be one of the reasons that Black women have worse breast cancer outcomes than other racial and ethnic groups. Lack of diversity among clinical trial participants means that new cancer treatments are being tested in groups of people that are not representative of the broader patient population that will receive these treatments if they are approved.
 “We need everyone appropriately represented because we want to make sure a therapy works the same way and the side effects are the same in different populations,” said Karen Winkfield, MD, executive director of the Meharry-Vanderbilt Alliance in Nashville, Tennessee. “Sometimes a medicine might work better in one population than another. We need to learn these things up front so we can give each patient the right medicine at the right time.”
“We need everyone appropriately represented because we want to make sure a therapy works the same way and the side effects are the same in different populations,” said Karen Winkfield, MD, executive director of the Meharry-Vanderbilt Alliance in Nashville, Tennessee. “Sometimes a medicine might work better in one population than another. We need to learn these things up front so we can give each patient the right medicine at the right time.”
 Up until recently, women of color have been largely left out of breast cancer research, including treatment trials and other types of studies that help doctors understand risk and risk reduction. “The majority of research in breast cancer screening, treatment, and hereditary susceptibility has been conducted on women with European ancestry,” said Lisa Newman, MD, of Weill Cornell Medicine and New York-Presbyterian in New York City. “We therefore face major gaps in knowledge. For example, we don’t know whether African American women might benefit from modified breast cancer screening recommendations, and we have an inadequate understanding of the genetics of triple-negative breast cancer.”
Up until recently, women of color have been largely left out of breast cancer research, including treatment trials and other types of studies that help doctors understand risk and risk reduction. “The majority of research in breast cancer screening, treatment, and hereditary susceptibility has been conducted on women with European ancestry,” said Lisa Newman, MD, of Weill Cornell Medicine and New York-Presbyterian in New York City. “We therefore face major gaps in knowledge. For example, we don’t know whether African American women might benefit from modified breast cancer screening recommendations, and we have an inadequate understanding of the genetics of triple-negative breast cancer.”
 “The reason we want diverse populations in clinical trials is that we want patients present with a range of genetic, social, economic, and geographic factors. We want all patients to benefit from clinical trials, and, when we assess new therapies, we want to understand how they will impact diverse populations,” said Lori Pierce, MD, of the University of Michigan and past president of the American Society for Clinical Oncology.
“The reason we want diverse populations in clinical trials is that we want patients present with a range of genetic, social, economic, and geographic factors. We want all patients to benefit from clinical trials, and, when we assess new therapies, we want to understand how they will impact diverse populations,” said Lori Pierce, MD, of the University of Michigan and past president of the American Society for Clinical Oncology.
Source: “Special Report: Increasing Racial Diversity in Breast Cancer Clinical Trials” (BreastCancer.org)
 “Clinical trials set the standards for breast cancer treatments, but barely include Black bodies…Which means that most breast cancer treatments have been and continue to be trialed on older white women,” says Ricki Fairley.
“Clinical trials set the standards for breast cancer treatments, but barely include Black bodies…Which means that most breast cancer treatments have been and continue to be trialed on older white women,” says Ricki Fairley.
“A treatment that works for an older, earlier stage white patient may not work the same for a young Black woman. The truth is, we can’t know without more research and data. In order to test how drugs work on Black bodies and keep Black Breasties from dying at higher rates, we need more Black women in clinical trials. But sadly, many Black women are never even offered clinical trial participation by their doctors.
This is a matter of life and death for Black women. We need to participate in clinical trials, if not for ourselves, for future generations of young, Black Breasties: our daughters, sisters, nieces and friends. Young Black women shouldn’t have to continue to rely on drugs that were not designed for them.”
See “Ricki Fairley, Co-Founder of TOUCH, The Black Breast Cancer Alliance Shares Why Clinical Trial Participation Will Help Black Women Beat Breast Cancer” on the Ebony website (2022)
Source: breastcancer.org
Every FDA-approved prostate cancer drug was tested in clinical trials
To look for better ways to care for people with prostate cancer, doctors create research studies involving volunteers, called clinical trials. Every FDA-approved drug was tested in clinical trials.
Clinical trials are used for all types and stages of prostate cancer. Many focus on new treatments to learn if a new treatment is safe, effective, and possibly better than the existing treatments. These types of studies evaluate new drugs, different combinations of treatments, new approaches to radiation therapy or surgery, and new methods of treatment.
Some clinical trials study new ways to relieve symptoms and side effects during treatment. Others study ways to manage the late effects that may happen a long time after treatment.
People who participate in clinical trials can be some of the first to get a treatment many years before it is available to the public.
Source: Prostate Cancer: About Clinical Trials (American Society of Clinical Oncology, 2021)
"We don't extend lives without research"
 “We don’t make advances, we don’t extend lives without participating in research,” says Andrew Armstrong, M.D., a prostate surgeon at Duke University. “We’re not happy with the way things are. We want them to be better and the only way to make them better is by studying them.”
“We don’t make advances, we don’t extend lives without participating in research,” says Andrew Armstrong, M.D., a prostate surgeon at Duke University. “We’re not happy with the way things are. We want them to be better and the only way to make them better is by studying them.”
Not all of these trials are successful, unfortunately. But many are and that’s why we are seeing men live longer and have better survivorship nowadays.”
Armstrong looks for biomarkers that will identify patients with prostate cancer who are at higher risk for a more aggressive clinical progression of the disease.
Source: Should Prostate Cancer Patients Consider a Treatment in Clinical Trials? (video, 2021)
The disparities in clinical trials significantly affect the efficacy of treatment for under-represented groups. This impact will only increase as the trend of personalized medicine continues and treatments like immunotherapy are explicitly tailored to one’s genes. Without sufficient data regarding a patient group, doctors have limited ability to predict how they may respond to treatment.
For example, a 2017 study found that some African Americans have lung tumors with a different gene expression than those found in white patients. This could impact the efficacy of specific therapies.
In the U.S., patients who enroll in cancer treatment trials tend to be younger, male, and white. This lack of diversity in clinical trials can lead to a cycle where new treatments are most effective for the most represented group. The results are not generalizable or misapplied to certain populations and perpetuate health disparities in the lung cancer continuum.
Source: “Lack of Diversity in Clinical Trials: A Patient’s Guide” (Lung Cancer Foundation of America)
It is no secret that there is a lack of diversity in clinical research. With fewer than five percent of all adults diagnosed with cancer participating in trials, the adverse effects of this disparity are magnified when it comes to the treatment and care of minority patients.
The disparities in clinical trials significantly impact the efficacy of treatment for underrepresented groups. This impact will only increase as the trend of personalized medicine continues and treatments like immunotherapy are explicitly tailored to one’s genotype. Without sufficient data regarding a patient group, doctors have limited ability to predict how they may respond to treatment.
For example, a found that some African Americans have lung tumors with a different gene expression than those found in white patients. This could impact the efficacy of specific therapies.
Source: “Lack of Diversity in Clinical Trials: A Patient’s Guide” (Lung Cancer Foundation of America)
Diversifying prostate cancer clinical trials essential for getting the right treatment to all men
Diverse clinical trials matter. Results obtained from diverse clinical trials help medical professionals and researchers understand how race and ethnicity affect prostate cancer risks and outcomes.
Since the majority of participants in clinical trials for prostate cancer are White men, there is little opportunity to study direct effects on People of Color.
Diversifying prostate cancer clinical trials is essential for getting the right treatment to all populations. Non-diverse clinical trials can result in a non-represented population experiencing negative outcomes, such as getting the wrong dose of a drug or receiving a treatment that won’t work as well for their particular needs.
Source: “Prostate Cancer Clinical Trials Need More Diversity” by Ashley Zlatopolsky on the Healthline website (March 18, 2022)
“You can imagine the shock of my family when we all learned that I had stage four lung cancer,” says Sheena. “My decision to participate in a clinical trial came as a result of my conversation with the oncologist.”
“Part of the challenges in the African American community is that we don’t have a lot of data because many African Americans don’t participate in clinical trials. I said yes, one of the things that I would love to share, with me being an African American woman, is how we respond to health care. I know a lot of it has to do with trust and believe me, I get that.”
“But when you think about your health, you read in Scripture that your body is your temple, so taking care of it and making sure that we find the right providers that can help us is very critical.”
A 2-minute video from the American Lung Association.
When We Tri(al): a campaign to increase Black participation in clinical trials


“The purpose of our When We Tri(al) movement is to help our Black community understand the importance of breast cancer science. Black women need to know that our breast cancer deserves special attention and we all together need to advance the science,” says Ricki Fairley, triple-negative breast cancer (TNBC) survivor and the Co-Founder and CEO of TOUCH, The Black Breast Cancer Alliance.
A 4-minute video from TouchBBCA.
Clinical Trials Representation

In eight clinical trials testing oral chemotherapy drugs for the treatment of breast cancer between 2009 and 2019, in which the race of the participants was recorded, less than six percent of the participants were Black or Hispanic women.
Black Americans make up more than 13% of the U.S. population. But in the clinical trials that led to FDA approval of four new breast cancer treatments in 2020, only 2% to 9% of participants were Black. Similarly, Hispanic or Latin Americans make up 18.5% of the U.S. population, but accounted for 0% to 9% of participants in those same trials.
One of these new treatments is a targeted therapy called Trodelvy, used to treat advanced-stage triple-negative breast cancer. Black women are twice as likely as White women to be diagnosed with triple-negative breast cancer in the United States. But only 7% of the Trodelvy trial participants were Black.
Source: “Why are people of color underrepresented in clinical trials?” at breastcancer.org

W=White 85.6%, B=Black 8.3%, A=Asian 4.8%, H=Hispanic 1.1%, AI=American Indian and Alaskan Native 0.2%
Among 93 clinical trials for breast, colorectal, lung, and prostate cancers from 2004 to 2017, lung cancer studies had the highest proportion of White and Asian participants and the lowest proportion of Black, Hispanic, and American Indian/Alaskan Native participants.
Source: Racial and Ethnic Disparities Among Participants in Precision Oncology Clinical Studies (2021)

Between 2009 and 2019, 21 clinical trials led to FDA approval of 12 oral chemotherapy agents for the treatment of Non–Small Cell Lung Cancer. Eleven of these trials reported on at least one race. In these 11 clinical trials, which had a total of 3,811 participants, 56% of the participants were Asian, 42% were White, and less than 2.5% were Black or Hispanic.

W=Whites 76%, A=Asians 8%, B=Blacks 3%, O=Other or multiple races 2%, AI=American Indian, Alaskan Native, Native Hawaiian or other Pacific Islander 1%, ?=Unknown 11%.
Source: “Race reporting and diversity in US food and drug administration (FDA) registration trials for prostate cancer; 2006-2020.” by M.P. Lythgoe et al. (2021)
Clinical Trials Barriers

In the United States, racial and ethnic minorities have been underrepresented in cancer clinical trials for decades, even when they have a similar or higher risk of the type of cancer being studied. Researchers have found that there are some common barriers that prevent people of color from participating in clinical trials. These include:
Not finding out about clinical trial opportunities. Many people of color don’t find out about clinical trial opportunities because their doctors don’t present them as an option. This can be a major barrier, because many people don’t know how to ask about, research, or find clinical trials on their own without a doctor’s support.
Overly strict eligibility criteria. Every clinical trial has guidelines about who is eligible to join to protect the safety of trial participants and ensure that they share certain characteristics, such as cancer type or previous treatments. But overly strict eligibility criteria have prevented many people from being able to enroll in clinical trials by excluding diseases that disproportionately affect people of color, such as high blood pressure (hypertension), diabetes, HIV, hepatitis B, and hepatitis C.
Travel and transportation. Clinical trial participants often have to travel to a clinical trial site for regular in-person visits which can be time-consuming and expensive. If you lack transportation, can’t take time off from work, or have family caregiving responsibilities, it can be more difficult to participate in a trial.
Out-of-pocket costs. Clinical trials usually pay for anything that is part of the trial, such as the study treatment you’ll receive, while health insurance usually covers routine care costs. But trial participants may have extra, out-of-pocket expenses such as parking, gas, taxis, airfare, and lodging that are not covered by the trial or health insurance. People may also face challenges with insurance coverage during the trial or lost income from time taken off work.
Lack of trust in the healthcare system. People of color may have personally experienced or observed discrimination in a healthcare setting. Or they may have received inferior care; research shows that Black and Hispanic women are less likely than white women to receive breast cancer treatment that adheres to medical guidelines.
All of these barriers contribute to the lack of diversity among clinical trial participants. But the barrier with the biggest impact may be that people of color simply aren’t being told about clinical trial opportunities or asked to participate. “If it’s not presented to you, how are you going to participate?” says Eleanor M. Walker, MD, director of breast radiation oncology for the Henry Ford Health System in Detroit, Michigan.
Read more at “Why are people of color underrepresented in clinical trials? in breastcancer.org’s “Special Report: Increasing Racial Diversity in Breast Cancer Clinical Trials.”
Clinical Trials Considering
Three big reasons to join a clinical trial
Reason one. When you take part in a clinical trial, you have a chance to receive treatment based on the latest research that is not yet available to others. Clinical trials are based on the best knowledge available for your kind of cancer.
Reason two. People in clinical trials get high-quality care. You’ll be carefully monitored throughout the study.
Reason three. When you take part in a clinical trial, you add to the world’s knowledge about cancer and help to improve cancer care for future generations. What doctors learn from you during the trial will help other people with cancer down the road.
A 2-minute video from the National Cancer Institute
Interested in joining a breast cancer clinical trial, but  feeling overwhelmed or don’t know where to start? Here are some common questions about the challenges people face in finding and participating in a clinical trial and some helpful tips on how to find trials and make participating easier.
feeling overwhelmed or don’t know where to start? Here are some common questions about the challenges people face in finding and participating in a clinical trial and some helpful tips on how to find trials and make participating easier.
For the Special Report: Increasing Racial Diversity in Breast Cancer Clinical Trials, breastcancer.org spoke with experts and clinical trial participants about why diversity in clinical research matters, and how you can overcome common barriers that may be preventing you from participating in a breast cancer clinical trial.
- When is the right time to consider a clinical trial?
- How do I start the process of looking for a clinical trial?
- What should I expect when applying to enroll in a clinical trial?
- What can I ask of the trial coordinators to make it easier for me to participate in a trial?
- What costs may be involved with participating in a clinical trial and who can help me navigate the financial and insurance issues?
- What risks are involved with joining a trial and what safeguards help protect participants?
- How can I find other women who have participated in clinical trials to talk with about their experiences?
- How can I get support and make sure I get my questions answered at my appointments related to enrolling in a clinical trial?
Questions to Ask Your Doctor about Treatment Clinical Trials

If you are thinking about taking part in a clinical trial, be sure to ask your doctor, “Is there a clinical trial that I can join?” If your doctor offers you a trial, here are some questions you may want to ask, such as:
How long will I be in the trial? What kinds of tests and treatments are involved? How will the doctor know if the treatment is working? How will I be told about the trial’s results? How long do I have to make up my mind about joining this trial? Who can I speak with about questions I have during and after the trial? Who will be in charge of my care? Is there someone I can talk to who has been in the trial?
Source: “Questions to Ask Your Doctor about Treatment Clinical Trials” (National Cancer Institute)
Steps to Find a Clinical Trial
Learn how to find the right clinical trial for you with the National Cancer Institute’s six-step guide:
Step 1: Gather Details about Your Cancer
Step 2: Find Clinical Trials
Step 3: Take a Closer Look at the Trials that Interest You
Step 4: Contact the Team Running the Trial
Step 5: Ask Questions
Step 6: Make an Appointment
A 2-minute video from the National Cancer Institute
“Clinical trials play a big role in our medical decision making. Simply put, you need to be represented for us to make a good decision based on your particular cancer and how it works in your body,” says Janine Harewood, M.D., an oncologist in Ft. Myers, Florida.
Some reasons why you should participate in clinical trials: you get first access to drugs which are not available in the general population as yet, you’re more likely to get frequent health checkups just because you need to be closely monitored, and it’s an opportunity to make a difference and help other patients gain from the information that we learn.”
“But for every good thing, it does come with risks. It’s a clinical trial because we don’t know everything. We’re trying to assess how the drug works, if it does work or if there any side effects.”
“The most common fear I hear from patients is that they won’t get the treatment when they’re on trial. Clinical trials today are not like they were. Now when clinical trials are designed, there’s the trial drug and then there’s the standard of care, not a placebo.”
“Clinical trials are always an option. Even if you’re not confident right now about going into a clinical trial and you’re comfortable with your treatment, there’s no harm in seeing what your options are.”
“I encourage you in the same way I would encourage my family. Please open yourself to the idea of a clinical trial and at least make sure that you get all the information so that you can make an informed decision.”
A 4-minute video from You and Lung Cancer.
Researchers need different people to take part in different clinical trials. For example, a particular trial may need volunteers with a certain type or stage of lung cancer, or of a certain age, sex or ethnicity.
The benefit of taking part in a clinical trial is that it allows you to try a drug treatment or procedure that is not yet available to the public. The risk is that you may experience unwanted side effects. The trial may benefit your health or it may not, but the knowledge that researchers gain will benefit people in the future.
Ask your doctor about joining a clinical trial. You can ask any time before or during treatment. You can leave a clinical trial at any time and you will still receive treatment for your lung cancer unless you want to stop that.
A 6-minute video from You and Lung Cancer and developed by A Breath of Hope Lung Foundation and Mechanisms in Medicine Inc. with support from pharmaceutical companies.

Page 1 of “Clinical Trial Options For Men With Prostate Cancer,” a 12-page brochure from Zero, the end of prostate cancer and Clovis Oncology, a pharmaceutical company
“Number one is what are the alternatives that I would have if I did not participate in the clinical trial? What are the standard of care therapies? Prostate cancer now has a vast menu. Many patients don’t necessarily even hear that,” says prostate cancer surgeon Andrew Armstrong, M.D., at the Duke University Cancer Center,
“It’s important to ask about risks. What have other patients experienced going into that study? What’s the evidence that it has helped people before? Why is this so promising?
Then, if you’re hearing about a trial and you’re making a decision to travel, sometimes asking questions about whether the trial will cover your lodging or transportation, gas, money, lodge, airport travel. Some trials do do that.”
A 2-minute video from the Patient Empowerment Network.
“I think sometimes there’s this misconception that clinical trials should only be utilized when there aren’t any other options,” says Rana R. McKay, M.D.
“Where in fact, I would say clinical trials should be an option to discuss every single time a treatment is being changed, because ultimately the goal is to make sure patients are living longer and living better. And making sure that clinical trials are an option on the table at every juncture is really a key step in that.”
McKay leads a prostate cancer clinic treating men diagnosed with aggressive prostate cancer and teaches at the University of California San Diego School of Medicine.
A 3-minute video from the Patient Empowerment Network.
“The easiest way to learn about clinical trials is to start start by asking the physician that’s treating you for your prostate cancer,” says prostate surgeon Yaw Nyame, M.D. “Oftentimes they’ll have resources and connections to the trials directly or the people who are administering them.”
“Other great sources are going to be patient advocacy networks. There are many of them for prostate cancer. These are great sources of finding out what clinical trials exist.”
Nyame treats kidney, prostate, bladder and testicular cancers at the Fred Hutchinson Cancer Center and teaches at the University of Washington School of Medicine.
“The trick is navigating all the information and knowing what trials are available for you, whether you qualify and that kind of thing can be difficult.”
A 4-minute video from the Patient Empowerment Network.
Clinical Trials Finding Govt



Learn how to find the right clinical trial for you with the National Cancer Institute’s six-step guide.
If you are thinking about joining a clinical trial as a treatment option, the best place to start is to talk with your doctor or another member of your health care team. Often, your doctor may know about a clinical trial that could be a good option for you. He or she may also be able to search for a trial for you, provide information, and answer questions to help you decide about joining a clinical trial.
Some doctors may not be aware of clinical trials that could be appropriate for you. If so, you may want to get a second opinion about your treatment options, including taking part in a clinical trial.
If you decide to look for trials on your own, the steps discussed here can guide you in your search.
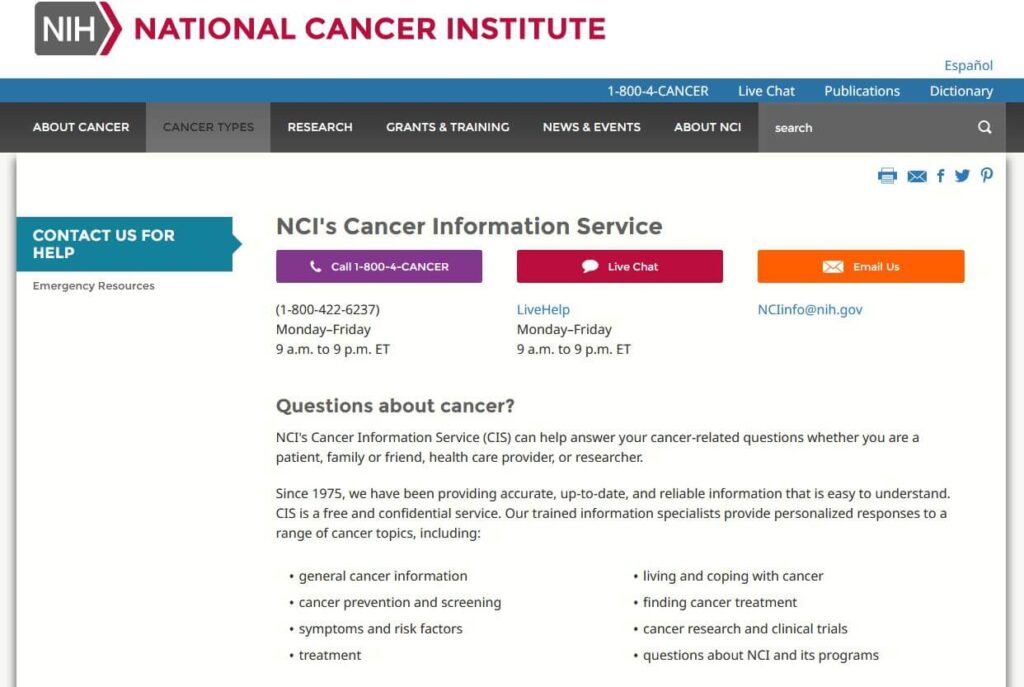
The NCI’s Cancer Information Service can also provide a tailored clinical trials search that you can discuss with your doctor. To reach them call 1-800-4-CANCER (1-800-422-6237) and select option 2. This is a free service. Keep in mind that the search results do not replace advice from your doctor.
Source: National Cancer Institute (2022)
ClinicalTrials.gov is a database of privately and publicly funded clinical studies conducted in all 50 states and in 221 countries.
The website provides current information about clinical research studies for patients, their families and caregivers, health care professionals, and the public.
Each study record includes a summary of the study protocol, including the purpose, recruitment status, and eligibility criteria. Study locations and specific contact information are listed to assist with enrollment.
Information on ClinicalTrials.gov is provided and updated by the organizations and people that sponsor and carry out the studies. Listing a study does not mean it has been evaluated by the U.S. Federal Government.
Clinicaltrials.gov is a free service of the National Institutes of Health (NIH) and is maintained by the National Library of Medicine (NLM).
For more information about using the database, visit clinicaltrials.gov

“If you decide to look for trials on your own, learn how to find the right clinical trial for you with the National Cancer Institute’s six-step guide:
- Step 1: Gather details about your cancer
- Step 2: Find clinical trials
- Step 3: Take a closer look at the trials that interest you
- Step 4: Contact the team running the trial
- Step 5: Ask questions
- Step 6: Make an appointment
The NCI’s Cancer Information Service can also provide a tailored clinical trials search that you can discuss with your doctor. To reach them call 1-800-4-CANCER (1-800-422-6237) and select option 2. This is a free service. Keep in mind that the search results do not replace advice from your doctor.
Source: National Cancer Institute (2022)
Clinical Trials Finding Groups
Cancer immunotherapy clinical trials are critical to bringing new and potentially lifesaving treatments to more patients with more types of cancer, and may represent the greatest hope for those currently facing the disease. Immunotherapy is increasingly available in clinical trials for early-stage cancers or as a first-line treatment option as clinical research rapidly progresses. Many patients, however, are not aware of recent breakthroughs in immunotherapy research and the growing opportunities to participate in new cancer clinical trials. Without this information, patients may find it difficult to identify cancer clinical trials that may be appropriate for them.
Our Cancer Immunotherapy Clinical Trial Finder will aid you in finding your answer to cancer. Understand the basics of cancer clinical trials, why clinical trials are so critical to our work, what things to consider about enrolling, and how to assist patients in finding clinical trials for which they may be eligible.
Source: Cancer Research Institute
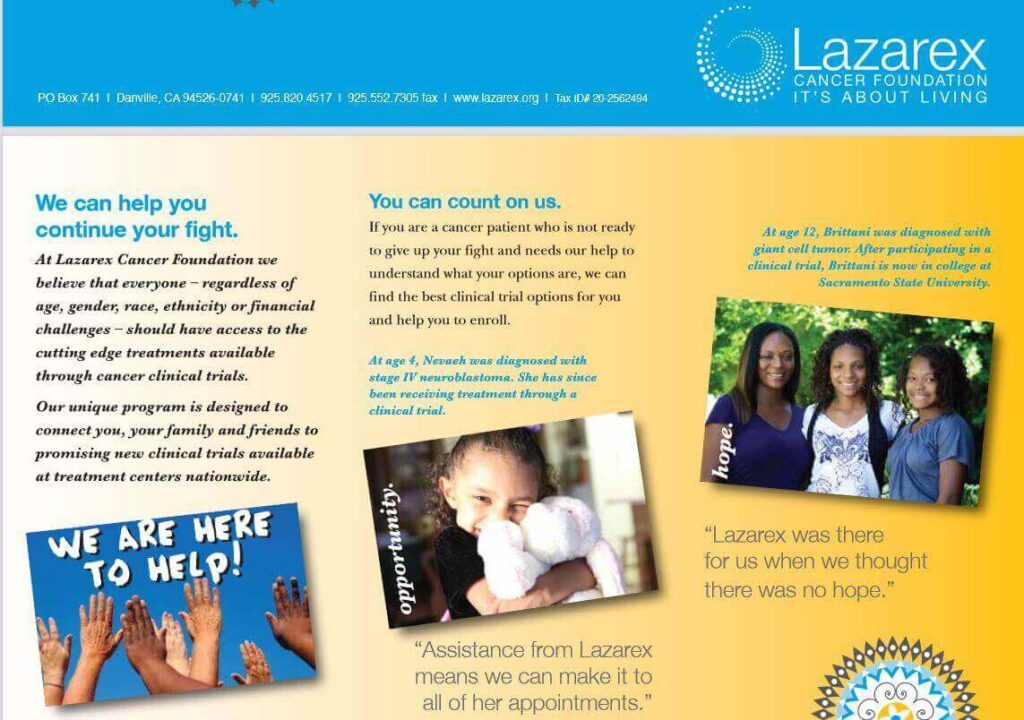
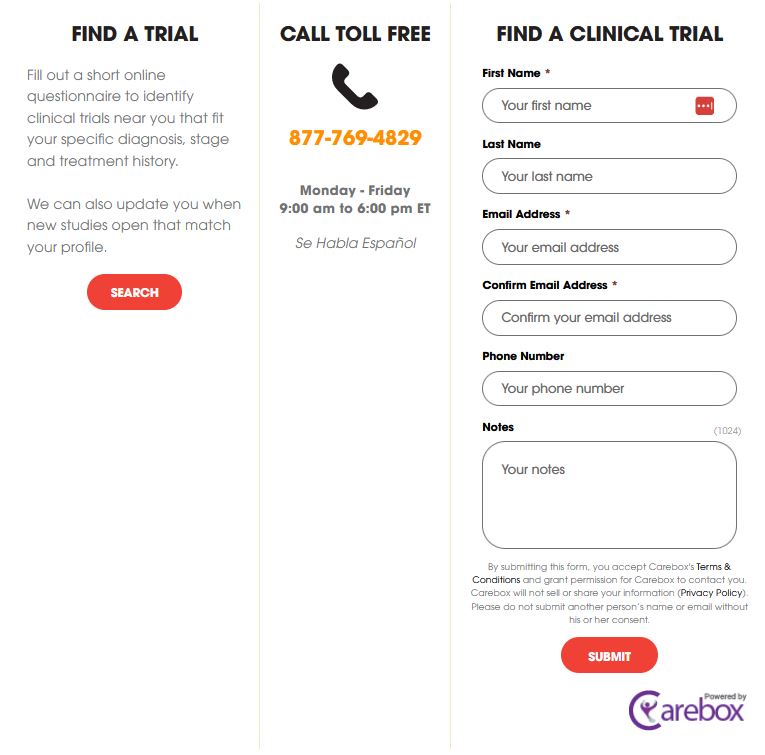
If you are a cancer patient who needs help identifying clinical trial options or needs financial assistance to attend a clinical trial, we’d like to hear from you. Our Patient Navigator can help you find the right clinical trial. We can also help you with the costs associated with participating in a clinical trial, including transportation and lodging.
For more information, email Lazarex or to speak with a Lazarex representative, call 925.820.4517.
Source: Lazarex Cancer Foundation

- Help individuals who are interested in breast cancer research find studies that are right for them.
- List all of the U.S-based trials on ClinicalTrials.gov and Cancer.gov that are currently looking for volunteers.
- Provide accurate information about why clinical trials are important and how they are structured.
- Help researchers and site coordinators connect more efficiently with volunteers who are interested in their studies.
- Help care providers and patient navigators find trials for patients.
Source: Breastcancertrials.org

Susan G. Komen® Breast Care Helpline
For more information about clinical trials, please call our Helpline at 1-877 GO KOMEN (1-877-465-6636) or email at clinicaltrialinfo@komen.org to connect with a trained specialist. Our caring and trained staff provide support and education about clinical trials to help people gain a better understanding of clinical trials.
The Helpline offers breast cancer clinical trial education and support, such as:
- Knowing when to consider a trial
- How to find a trial
- How to decide which trial is best
- What to expect during a trial
- Information about clinical trial resources
Find Trials That May Be Right For You: Breast cancer patients at any stage can join a clinical trial. Breast cancer clinical trials study prevention, new screening tests and treatment options, as well as quality of life issues.
If you have early or locally advanced breast cancer, find a clinical trial
If you have metastatic breast cancer, find a clinical trial
More at Susan G. Komen

Our Cancer Immunotherapy Clinical Trial Finder will aid you in finding your answer to cancer. Understand the basics of cancer clinical trials, why clinical trials are so critical to our work, what things to consider about enrolling, and how to assist patients in finding clinical trials for which they may be eligible.
Source: Cancer Research Institute

Get matched to a prostate cancer clinical trial that’s right for you! Print out your results to discuss with your treatment team, or contact the study coordinators directly. Patients are matched to clinical trials by Antidote, a U.S. and U.K. firm that recruits volunteers for clinical trials.
Go to “Find a clinical trial” at Zero, the end of prostate cancer.

A free, over-the-phone service that helps Black or African American (AA) cancer patients learn more about clinical trials. The Peer Clinical Trials Support Program matches interested patients with a peer — a Black or African American cancer patient or survivor with experience participating in a cancer clinical trial.
Patients have the opportunity to discuss their fears, questions, and concerns with a knowledgeable and empathetic guide, and hear from someone of a similar background who has “been there, done that.”
Source: Cancer Support Community
Clinical Trials Brochures